Laparoscopic total mesorectal excision (TME) with electric hook for rectal cancer
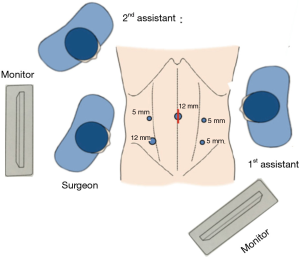
Positions of the patient, cannulas and the surgical team
The patient should be in steep Trendelenburg position and tilted right side down. The surgeon stands on the patient’s right side, the first assistant on the left side, and the second assistant (camera operator) on the left side of the surgeon. The main monitor is placed near the patient’s left shoulder, and the second monitor is placed behind the surgeon. Five cannulas (2 mm × 12 mm, 3 mm × 5 mm) are placed as shown in Figure 1.
Procedures
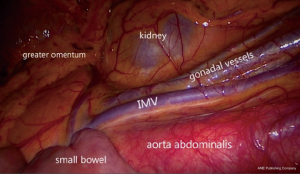
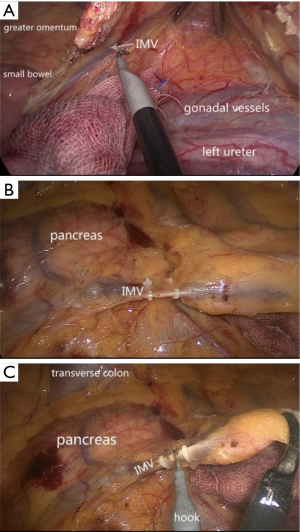
The small bowel loops are placed in the right side to expose the duodenum and the inferior mesenteric vein (IMV) (Figure 2).
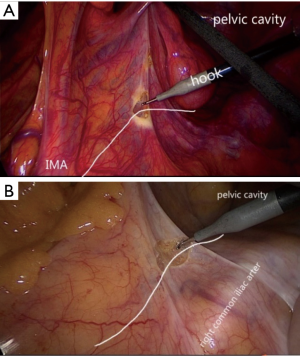
Surgeon must identify the tumor location firstly. The assistant should grasp the pedicle of superior rectal vessels and use an intestinal grasper to push the rectum ventrally and laterally. The promontory should be confirmed, so the surgeon can use the hook to incise the peritoneum at the level of promontory (Figure 3).
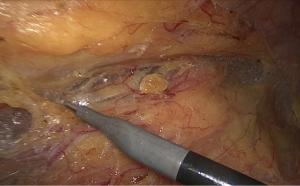
The surgeon should move to cephalad dissection. While cutting the subperitoneal connective, you should avoid damaging the hypogastric nerves (Figure 4).
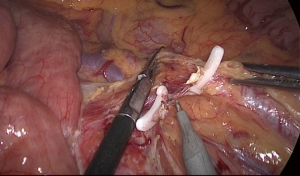
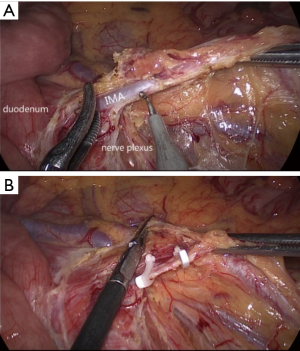
Incision of peritoneum is continued up to the origin of the inferior mesenteric artery (IMA). The surgeon and the assistant should recognize the nerves, the ureter, and the gonadal vessels, and you should also prevent the injuries to them (Figure 5). Two absorbable clips are required to occlude the origin of IMA, and then the IMA should be cut between these two clips (Figure 6).
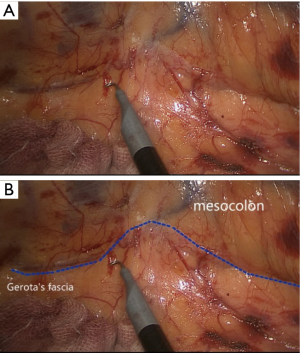
The dissection between the mesocolon and the retroperitoneum is advanced laterally and cephalad. Continuing to divide the adipose tissues, in order to create the Gerota’s fascia, which is a fibrous membrane covering the left kidney (Figure 7). Then the IMV and the pancreas will arise (Figure 8A). As same as the IMA, the adipose tissues surrounding the IMV need to be cleaned carefully, and two or more clips are required to occlude the IMV (Figure 8B,C).
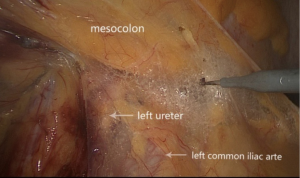
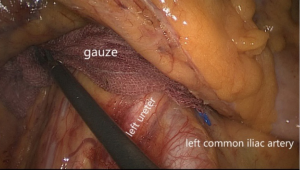
Following the cephalad dissection, you come back to the posterior dissection of the rectum. Surgeon and assistant should avoid doing harm to the left ureter and the left common iliac arte (Figure 9).
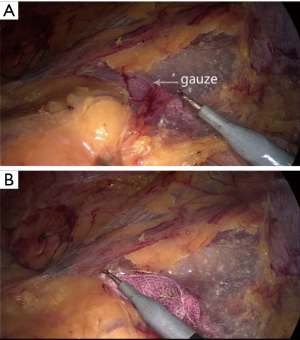
Once you have separated the mesocolon and the left common iliac arte, a gauze can be stuffed into the gap between them, in order to be the sign in the next step (Figure 10).
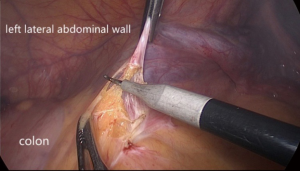
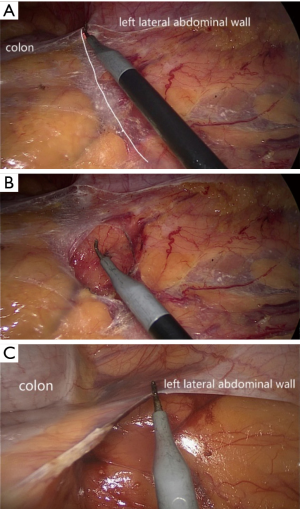
The assistant picks the paracolic sulci peritoneum by the left hand and the surgeon picks the mesocolon, in order to keep the tension (Figure 11). Traction is very important. Surgeon must be patient and careful to avoid damaging the left common iliac arte and the left ureter. Continuing cutting the paracolic sulci peritoneum until the gauze appears (Figure 12), and incision of peritoneum is continued up to the splenic flexure (Figure 13).
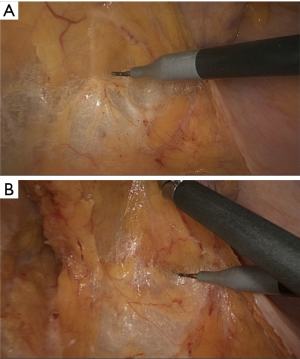
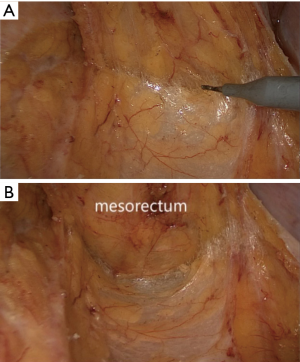
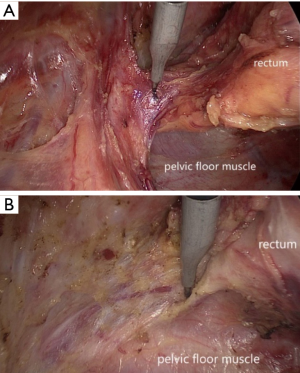
Then the surgeon can move to the posterior dissection of the rectum. The assistant should extend the fibrous tissues between the mesorectum and the retroperitoneum, in order to keep the sufficient traction. The rectal fascia propria can be created so that the surgeon can continue the following dissection. The prehypogastric nerve on both sides, the median or lateral sacral vessels should be protected (Figures 14,15).
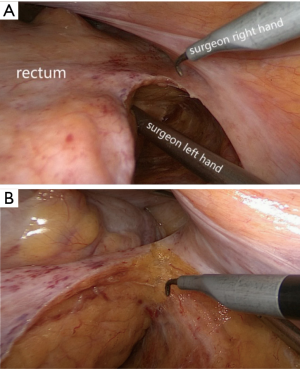
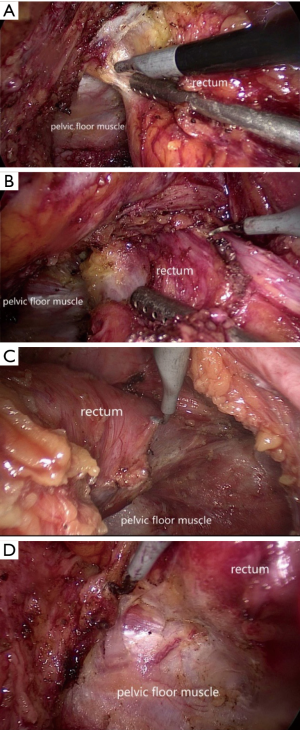
The lateral dissection on the left side and the right side is similar (Figures 16,17). The surgeon now incises the peritoneum carefully, avoiding damaging the pelvic nerve plexus, the neurovascular bundle (NVB) and the seminal vesicle.
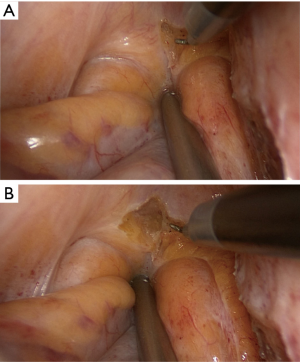
The surgeon could use the hook to open the peritoneal reflection. The assistant should push up the urinary bladder by one of his hand, to avoid the damage with bladder. The surgeon should try his best to extend the fibrous tissues between the seminal vesicle and the rectum (Figure 18).
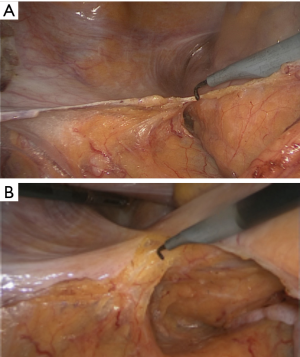
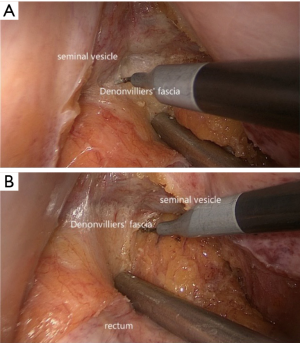
There is a fascia called “Denonvilliers’ fascia”, the fibrous tissues between the rectum and the seminal vesicles, the prostate, and the NVB (Figure 19).
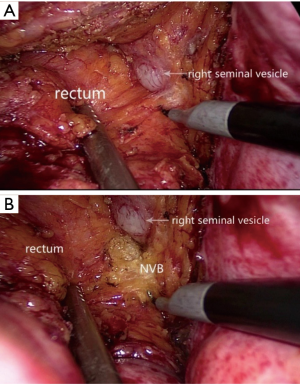
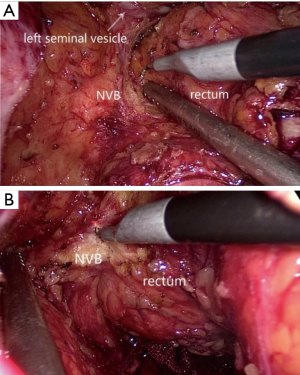
The surgeon and assistant should pay attention to the NVB on the both side, preventing to enter into them. The NVB must be everted from the rectum (Figures 20,21).
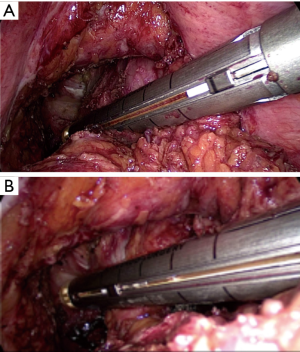
The dissection reaches the pelvic floor, and the so-called lateral ligament is created both in left and right anterolateral corner (Figure 22). Cut them off and clean the mesorectum to advance it to obtain a sufficient distal margin (Figure 23).
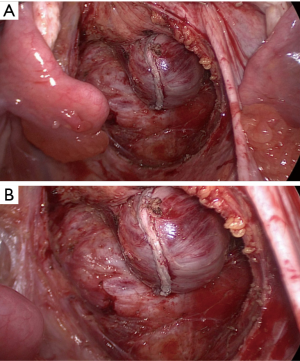
Once the surgeons have finished the dissection, some medical instruments can be used to divide the rectum (Figure 24). Then we can see the rectal stump and check it (Figure 25). Following to take the tumor from the abdomen, anastomosis is performed with either a double-stapling technique.
Conclusions
Laparoscopic total mesorectal excision (TME) with electric hook for rectal cancer is described. Comparing with ultrasound knife, the advantage of electric hook is obvious. Firstly, less smog will be produced if the electric hook is used within 2 seconds. Secondly, by using the electric hook, surgeon and assistants can find the clearer dissectible layer. Last but not least, tissue could be mobilized with the electric hook by sharp dissection instead of blunt dissection so that surgeon can prevent some unnecessary damage, such as hemorrhage and perforation.
Laparoscopy surgery with electric hook requires cooperation between the surgeon, first assistant surgeon and second assistant surgeon. Keeping the sufficient traction is important and necessary, which could help the surgeon recognize the correct layer and the organs, including the IMA, the IMV, the autonomic nerves, left ureter, left gonadal vessels, and pancreas (Figure 26).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2017.04.10). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chen G, Zhang RX, Xiao ZT. Laparoscopic total mesorectal excision (TME) for rectal cancer. Asvide 2017;4:204. Available online: http://www.asvide.com/articles/1514
Cite this article as: Chen G, Zhang RX, Xiao ZT. Laparoscopic total mesorectal excision (TME) with electric hook for rectal cancer. J Xiangya Med 2017;2:44.