
Statin pretreatment and presentation patterns in patients with acute coronary syndromes
Introduction
Statins reduce cardiovascular events in patients with hypercholesterolemia (1). This benefit could be related to atherosclerotic plaque stabilization at coronary level (2).
It has recently been observed that the type of presentation of acute coronary syndromes (ACS) could be conditioned by statin therapy: patients treated with statins would be less likely to develop ST elevation myocardial infarction (STEMI, more associated with total occlusion of the culprit vessel and greater amount of myocardial necrosis) than the other forms, non-STEMI (NSTEMI) and unstable angina (UA) (3). In other words, statins may be protective of STEMI, if any ACS develops.
However, patients who present STEMI are younger and have lesser history of coronary artery disease than other forms of ACS, they receive fewer statins at lower doses. This situation must to be taken into account because it is a strong confounder. Alternatively, statins may protect not only from STEMI but also from total myocardial infarction (STEMI + NSTEMI) favoring presentation as UA (4). The aim of this study was to analyze whether there is an association between previous use of statins and the presentation of ACS, including STEMI and acute myocardial infarction (AMI).
Methods
It was analyzed a retrospective cohort of 1,322 patients hospitalized for ACS between 2014 and 2016. They were classified as STEMI [247], NSTEMI [461] or AU [614] according to the 3rd universal definition of myocardial infarction (5) using high-sensitive cardiac T troponin with upper reference limit =14 ng/L representing the 99th percentile for this technique. Information of coronary risk factors, prior history of myocardial infarction or previous revascularization, chronic angina, and use of statins prior to admission (considering high doses when receiving at least atorvastatin 40 mg or rosuvastatin 20 mg), and other drugs that might condition the presentation of ACS, such as aspirin and beta-blockers, were collected. The protocol was approved by the institutional ethics committee
Statistical analysis
Values are expressed as mean ± standard deviation or median and interquartile range and they were compared by parametric tests or Kruskal Wallis as appropriate. Categorical variables were compared with the simple chi square test with Yates correction, chi square trend or multiple chi-square. To assess the effect of previous statins on the presentation of ACS, logistic regression analysis and propensity score (weighting) were performed. The program used (STATA/SE 11.2 for Windows) rejected the variable “previous angioplasty” among the variables of the propensity score model by collinearity (all patients with previous angioplasty received statins).
Results
The mean age was 67±12 years and 1,001 subjects (76%) were male. Clinical characteristics in the three types of ACS were compared in Table 1.
Table 1
| Variable | STEMI [247] | NSTEMI [461] | UA [614] | P |
|---|---|---|---|---|
| Age | 64±11 | 68±13 | 68±11 | 0.0001 |
| Female | 48 (20%) | 105 (23%) | 168 (27%) | 0.0032 |
| Hypertension | 142 (57%) | 297 (64%) | 439 (71%) | 0.0001 |
| Hypercholesterolemia | 161 (64%) | 369 (80%) | 475 (77%) | <0.0001# |
| Smoking | 172 (69%) | 278 (60%) | 394 (64%) | 0.054 |
| Diabetes | 41 (16%) | 105 (22%) | 141 (22%) | 0.06 |
| Familiar history | 52 (20%) | 89 (19%) | 162 (26%) | 0.018 |
| Prior AMI | 41 (16%) | 111 (24%) | 185 (30%) | 0.014# |
| Prior PCI | 36 (14%) | 124 (27%) | 249 (40%) | <0.0001# |
| Prior coronary surgery | 11 (4%) | 47 (10%) | 82 (13%) | 0.001/0.06# |
| Statins | 77 (31%) | 189 (40%) | 335 (54%) | <0.0001# |
| High dose statins | 21 (9%) | 49 (11%) | 117 (19%) | <0.0001# |
| Aspirin | 86 (35%) | 206 (46%) | 358 (59%) | <0.0001# |
| Beta blockers | 63 (26%) | 181 (40%) | 289 (48%) | 0.005# |
Multiple chi square. #, chi square trend. ACS, acute coronary syndrome; STEMI, ST elevation myocardial infarction; NSTEMI, non-STEMI; UA, unstable angina; AMI, acute myocardial infarction.
Patients with UA were older, more women and they had more coronary risk factors and cardiovascular history than the others.
There was a clear trend towards greater use of statins, aspirin and beta blockers in UA patients, followed by NSTEMI and STEMI (Figure 1).
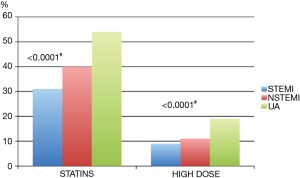
On the other hand, patients receiving statins (45%) had more coronary risk factors and cardiovascular events too, but less STEMI, NSTEMI and AMI compared with those statins naive (Table 2 and Figure 1).
Table 2
| Variable | Statins [601] | Statins naive [721] | P |
|---|---|---|---|
| Age | 68±11 | 66±12 | <0.05 |
| Female | 127 (21%) | 195 (27%) | <0.05 |
| Hypercholesterolemia | 530 (88%) | 401 (56%) | <0.001 |
| Hypertension | 462 (77%) | 479 (39%) | <0.001 |
| Diabetes | 125 (25%) | 142 (20%) | <0.02 |
| Prior AMI | 211 (35%) | 126 (17%) | <0.001 |
| Prior PCI | 283 (47%) | 126 (17%) | <0.001 |
| Prior coronary surgery | 94 (16%) | 46 (6%) | <0.001 |
| Chronic angina | 53 (9%) | 34 (5%) | <0.05 |
| ACS type | |||
| AMI | 267 (44%) | 442 (61%) | <0.001 |
| STEMI | 78 (13%) | 170 (23%) | <0.001 |
| NSTEMI | 189 (31%) | 273 (38%) | <0.02 |
| UA | 335 (56%) | 280 (39%) | <0.001 |
AMI, acute myocardial infarction; STEMI, ST elevation myocardial infarction; NSTEMI, non-STEMI; UA, unstable angina.
In logistic regression analysis (Table 3), pre-treatment with statins was statistically associated with a lower incidence of STEMI and AMI and higher incidence of UA as a form of presentation of ACS. The same was seen with pre-treatment with aspirin but not with beta-blockers to predict AMI.
Table 3
| Parameter | STEMI | AMI | |||||
|---|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | P (>|Z|) | Odds ratio | 95% CI | P (>|Z|) | ||
| Age | 0.986 | 0.973–0.999 | 0.0364 | 1.002 | 0.992–1.013 | 0.627 | |
| Gender (male) | 1.515 | 1.055–2.176 | 0.0246 | 1.617 | 1.234–2.120 | 0.0005 | |
| Hypertension | 0.672 | 0.486–0.927 | 0.0156 | 0.764 | 0.578–1.010 | 0.0583 | |
| Hypercholesterolemia | 0.852 | 0.612–1.185 | 0.3417 | 0.810 | 0.613–1.069 | 0.1371 | |
| Smoking | 1.474 | 1.079–2.015 | 0.0149 | 1.035 | 0.814–1.315 | 0.7785 | |
| Diabetes mellitus | 0.860 | 0.581–1.273 | 0.4525 | 1.002 | 0.756–1.328 | 0.9901 | |
| Family history | 0.818 | 0.572–1.171 | 0.2729 | 0.743 | 0.565–0.978 | 0.0342 | |
| Prior MI | 0.921 | 0.612–1.385 | 0.6914 | 1.032 | 0.775–1.375 | 0.8283 | |
| Prior angioplasty | 0.487 | 0.317–0.746 | 0.001 | 0.567 | 0.426–0.754 | <0.0001 | |
| Prior coronary surgery | 0.579 | 0.299–1.121 | 0.1051 | 0.785 | 0.533–1.154 | 0.2187 | |
| Chronic angina | 0.099 | 0.020–0.482 | 0.0042 | – | – | – | |
| Prior statins | 0.701 | 0.500–0.981 | 0.0385 | 0.729 | 0.561–0.947 | 0.0195 | |
| Prior aspirin | – | – | – | 0.730 | 0.559–0.952 | 0.0203 | |
| Prior beta blockers | – | – | – | 0.924 | 0.712–1.198 | 0.5495 | |
STEMI, ST elevation myocardial infarction; AMI, acute myocardial infarction.
In order to analyze the effect of statins in such different samples, the propensity score was used in order to obtain more comparable samples. After adjustment by propensity score, statin therapy continued to be independently associated with a lower incidence of AMI: propensity score weighting (IPTW) [odds ratio (OR) =0.739, 95% CI: 0.588–0.922, P<0.01].
Discussion
ACS usually occurs as a result of a rupture of an atherosclerotic plaque in the coronary arteries. Cholesterol plays an important role in the genesis and frailty of this plaque.
Several studies suggest that pretreatment with statins reduces the likelihood of presenting as STEMI in the event of an ACS, probably because of a pleiotropic effect on plaque stabilization (6). However, as evidenced in our study and in previous ones, patients pretreated with statins are different from others, which hinder the comparison between groups.
Statin therapy is more frequently used for secondary prevention (after a cardiovascular event) than for primary prevention. It is not surprising that patients with prior myocardial infarction or coronary revascularization receive more statins than those at lower risk (7).
In our population, we observed more use of previous statins in UA, followed by NSTEMI and STEMI respectively. These may be related to prior cardiovascular events, because the same pattern was observed with other protective drugs, as aspirin or beta-blockers.
We hypothesized that previous use of statins could protect not only STEMI but also the whole AMI (STEMI and NSTEMI), and this was the basis of our analysis.
It is already stated in introduction, since this was a retrospective analysis we needed a special statistical treatment for the groups to be comparable. Logistic regression is aimed to get a better balance of the variables, logistic regression controls the confounder effect of several variables, but it not makes comparable samples.
The propensity score is so the right method to control sample difference bias. However, one important variable as prior coronary angioplasty could not be taken into account due to high collinearity between use of statins and angioplasty. So, the propensity score did not take this variable to make more comparable the samples. Anyway, among UA patients without previous angioplasty, chronic statin use was significant more frequent than the others.
In our study, the use of statins was independently associated with less AMI and UA as presentation pattern of ACS, both by multiple logistic regression and by propensity score analysis. Moreover, prior aspirin use followed the same pattern, but not the prior use of beta-blockers.
Gottlieb et al. (3) analyzed data from the ACSs survey in large population in Israel and they found similar results using propensity score too: STEMI had lesser previous statins than NSTEMI and UA, but they did not analyze total AMI. Even more, statin use was better correlated with type of ACS than cholesterol level at admission. Ndrepepa et al. (4) observed at cath lab less ACS among patients receiving chronic statins. Statin intolerance has recently been observed to be associated with a poor prognosis (8) and this may be related to lack of benefits of these drugs. Patients pretreated with statins before STEMI would have a better outcome (9) and lower in-hospital and out-of-hospital mortality rate (10,11).
Limitations
the main weak of the study is, as common is this type of studies, to have non-comparable samples, which introduce a bias. Although bias could not be deal with statistics, propensity score technic helps with it. The low percentage of STEMI and high doses of statins prevented a more specific analysis in these subgroups. Another problem is the impossibility to score by previous coronary angioplasty.
Conclusions
Pretreatment with statins was associated with a more benign presentation in ACSs, more like UA (without elevation of biomarkers) than with AMI. This could be a way of coronary atherosclerotic plaque’s stabilization.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2017.08.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chou R, Dana T, Blazina I, et al. Statins for Prevention of Cardiovascular Disease in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2016;316:2008-24. [Crossref] [PubMed]
- Takata K, Imaizumi S, Zhang B, et al. Stabilization of high-risk plaques. Cardiovasc Diagn Ther 2016;6:304-21. [Crossref] [PubMed]
- Gottlieb S, Kolker S, Shlomo N, et al. Association between statin treatment and LDL-cholesterol levels on the rate of ST-elevation myocardial infarction among patients with acute coronary syndromes: ACS Israeli Survey (ACSIS) 2002-2010. Int J Cardiol 2016;210:133-8. [Crossref] [PubMed]
- Ndrepepa G, Fusaro M, King L, et al. Statin pretreatment and presentation patterns in patients with coronary artery disease. Cardiol J 2013;20:52-8. [Crossref] [PubMed]
- Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol 2012;60:1581-98. [Crossref] [PubMed]
- Otsuka F, Hibi K, Kusama I, et al. Impact of statin pretreatment on the incidence of plaque rupture in ST-elevation acute myocardial infarction. Atherosclerosis 2010;213:505-11. [Crossref] [PubMed]
- Moran L, Fugate T, Xiang Y, et al. Statin pretreatment is protective despite an association with greater coronary artery disease burden in patients presenting with a first ST-elevation myocardial infarction. Prev Cardiol 2008;11:21-5. [Crossref] [PubMed]
- Serban MC, Colantonio LD, Manthripragada AD, et al. Statin Intolerance and Risk of Coronary Heart Events and All-Cause Mortality Following Myocardial Infarction. J Am Coll Cardiol 2017;69:1386-95. [Crossref] [PubMed]
- Mytas D, Zairis M, Karanasos A, et al. Effect of statin pretreatment on the outcome of ST-segment elevation myocardial infarction in patients without prior history of coronary artery disease. Hellenic J Cardiol 2013;54:422-8. [PubMed]
- Lev EI, Kornowski R, Vaknin-Assa H, et al. Effect of previous treatment with statins on outcome of patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. Am J Cardiol 2009;103:165-9. [Crossref] [PubMed]
- Oduncu V, Erkol A, Kurt M, et al. The prognostic value of very low admission LDL-cholesterol levels in ST-segment elevation myocardial infarction compared in statin-pretreated and statin-naive patients
Cite this article as: Trivi M, Henquin R, Costabel J, Conde D. Statin pretreatment and presentation patterns in patients with acute coronary syndromes. J Xiangya Med 2017;2:65.


