Cardiac surgery in sub-Saharan Africa: a report of 3-year experience at the Douala General Hospital
Introduction
Cardiovascular diseases (CVDs) are the leading cause of mortality in the world (1). There is an increasing trend in Sub-Saharan Africa (SSA) in the last decade, with about 35 million people being affected. It is estimated that CVDs cause about 1 million deaths, representing 22% of mortality worldwide (1).
Some of these cardiac diseases require surgical management. In the absence of sufficient infrastructures and adequate technical platforms in low-income settings, patients are referred abroad. These transfers have both financial and social implications for African nations and the family of the patients (2).
In 1985, open heart surgery was started in Yaoundé—the political capital of Cameroon, in collaboration with the French (3). In 2008, a similar collaboration was established with the Belgians (4). In 2012, cardiac surgery was started in the General Hospital of Douala (DGH)—the economic capital of Cameroon, in collaboration with the free University of Bruxelles and Derluyn foundation. This North-South collaboration with the DGH known as the “Cardiac surgery program” has carried out five heart surgery missions. Little is known about the profile of heart diseases seen, surgical uptake, and outcome of this programme. This work aimed at reporting the experience of the first three years of this programme at the DGH.
Methods
Ethical statement
This work was approved by the institutional review board of the Douala General Hospital (DGH) (Ref. No. 038AR/MINSANTE/HGD/DM/02/16). We carried out this work in accordance with the declarations of Helsinki. We report this work according to the Standard for Reporting Observational Study (STROBE) checklist.
Study design and setting
We carried out a cross-sectional descriptive study in the cardiology unit, cardiovascular intensive care unit, and in the surgical unit of DGH from October 2012 to November 2015. We reviewed (retrospectively) the medical files of all patients with a heart disease, and who had an indication for heart surgery. We excluded files with incomplete key information (type of heart disease). The DGH is a tertiary health institution located in the economic capital of Cameroon (Political capital—Yaounde), SSA. It also serves as a teaching hospital, and has a catchment population of over three million inhabitants. It also receives referrals from the Central African sub-region.
Participants, source of data, and variables
These were all patients of both sex, with a heart disease requiring surgery, seen in the cardiology unit during the “Cardiac surgery programmes”. Patients were recruited from their case records. We excluded incomplete records (nature of heart disease not recorded). We collected information on the age, sex, city of origin, past medical history, symptoms and signs at presentation, nature of heart disease, surgical procedure (yes/no), type of procedure, reason for no procedure, post-procedure complications, and fatal outcome.
Sample size and power
We describe the initial 3-year experience of cardiac surgery at the DGH. All eligible cases were considered for this report.
Statistical analysis
Data were analyzed using the software EPI Info Version 3.1 (Centers for Disease Control and Prevention, Atlanta, Georgia, USA). We present qualitative data as frequencies and percentages. Age is presented as mean ± standard deviation (SD).
Results
A total of 45 patients with heart diseases who had an indication for surgery were retained for this study. There were 23 women and 22 men. Of these, 27 patients benefited from surgical intervention. Their mean age was 41±18 years (range, 14 to 85 years). Demographic and clinical characteristics are shown in Table 1. Most patients (42.2%) lived in Douala. Hypertension was the most frequent medical history reported by 16 (35.6%) patients. Dyspnea was reported by 8 (17.8%) patients. Heart murmur was the most frequent physical finding heard in 29 (64.4%) patients. Thirteen (28.9%) patients were in congestive heart failure. The distribution of the different heart diseases is shown in Table 2. Valvular heart diseases were the most frequent, seen in 32 (71.1%) patients, which were predominantly rheumatic heart diseases (RHD) seen in 25 (55.6%) patients. Aortic valvular involvement represented 28.8% of valvular heart diseases with mitral valve involvement accounting for 22.3% of cases. Infective endocarditis was found in 4.4% of cases. Of the 45 patients, 13 (29.6%) had congenital heart diseases, with the most frequent being persistent ductus arteriosus (9.1%), followed by atrial septal defect and coarctation of the aorta, which all accounted for 6.8% of cases. Three (6.6%) patients presented with atrial tumors.
Table 1
| Variable | Frequencies | Percentage (%) |
|---|---|---|
| Residence | ||
| Douala | 19 | 42.2 |
| Yaoundé | 15 | 33.3 |
| Others | 11 | 24.4 |
| Past history | ||
| Hypertension | 16 | 35.6 |
| Valvular heart disease | 5 | 11.1 |
| Tobacco consumption | 4 | 8.9 |
| Congenital heart disease | 3 | 6.7 |
| Diabetes | 3 | 6.7 |
| Mitral valve plasty | 2 | 4.4 |
| Functional signs | ||
| Dyspnea | 8 | 17.8 |
| Angina | 4 | 8.9 |
| Fever | 2 | 4.4 |
| Murmur | 1 | 2.2 |
| Physical signs | ||
| Heart murmur | 29 | 64.4 |
| Congestive heart failure | 13 | 28.9 |
| Left heart failure | 5 | 11.1 |
| Right heart failure | 1 | 2.2 |
| Hepatomegaly | 5 | 11.1 |
| Systemic inflammation response syndrome | 3 | 6.7 |
| Lower limb edema | 3 | 6.7 |
| Ascites | 1 | 2.2 |
| Hepatojugular reflux | 1 | 2.2 |
Table 2
| Diseases | Frequencies | Percentage (%) |
|---|---|---|
| Rheumatic valve disease | ||
| Mitral stenosis | 3 | 6.7 |
| Mitral insufficiency | 3 | 6.7 |
| Mitral valve disease | 2 | 4.4 |
| Aortic stenosis | 1 | 2.2 |
| Aortic insufficiency | 9 | 20.0 |
| Aortic valve disease | 2 | 4.4 |
| Tricuspid insufficiency | 1 | 2.2 |
| Degenerative valve disease | ||
| Calcified aortic stenosis | 2 | 4.4 |
| Dystrophic valve disease | ||
| Mitral and aortic insufficiency | 1 | 2.2 |
| Endocarditis | ||
| Mitral insufficiency | 2 | 4.4 |
| Congenital heart diseases | ||
| Patent ductus arteriosus | 4 | 8.9 |
| Coarctation of aorta | 3 | 6.7 |
| Atrial septal deflect | 3 | 6.7 |
| Bicuspid aortic valve | 1 | 2.2 |
| Ventricular septal deflect | 1 | 2.2 |
| Tetralogy of Fallot | 1 | 2.2 |
| Tumors | ||
| Right atrium | 2 | 4.4 |
| Left atrium | 1 | 2.2 |
| Others | ||
| Aortic aneurysm | 5 | 11.1 |
| Pericarditis | 2 | 4.4 |
| Valsalva sinus aneurysm | 1 | 2.2 |
| Aortic dissection | 1 | 2.2 |
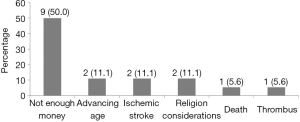
Of the 45 patients, 27 (60%) underwent cardiac surgery, with 3 (11.1%) closed-heart surgeries and 24 (88.9%) open-heart surgeries. The surgical procedures are summarized in Table 3. Valve replacement was the most common type of surgery carried out in 12 (44.5%) patients, followed by correction of congenital heart diseases in 9 (33.3%) patients. The distribution of patients based on their reasons for not undergoing surgery is shown in Figure 1. The cost of surgery was the limiting factor in 9 (50%) patients, followed by advanced age, recent stroke, and religious constraints. Early in-hospital post-surgical complications are shown Table 4. Two patients had infection, and two with massive hemo-pericardium. Conduction disorders and thromboembolic events were present in one patient each. Among the 27 patients operated, two died in the hospital (intra-hospital mortality rate: 7.4%). No late complication has been recorded.
Table 3
| Procedure(s) | With prosthesis | Without prosthesis | Total (%) | |
|---|---|---|---|---|
| Interventions | BP | MP | ||
| Mitral valve replacement | 1 | 2 | – | 3 (11.1) |
| Aortic valve replacement | 1 | 3 | – | 4 (14.8) |
| Mitral and aortic valve replacement | 0 | 1 | – | 1 (3.7) |
| Mitral annuloplasty | – | – | 1 | 1 (3.7) |
| Mitral valve replacement + aortic annuloplasty | 1 | – | – | 1 (3.7) |
| Mitral valve replacement + tricuspid annuloplasty | 1 | – | – | 1 (3.7) |
| Ventricular septal deflect closure | – | – | 3 | 3 (11.1) |
| Atrial septal deflect closure | – | – | 3 | 3 (11.1) |
| Ductus arteriosus closure | – | – | 3 | 3 (11.1) |
| Benthal surgery | 2 | – | 2 (7.4) | |
| Tyron/Davis surgery | – | – | 1 | 1 (3.7) |
| Myxoma cure | – | – | 2 | 2 (7.4) |
| Axillary-femoral bypass | – | – | 2 | 2 (7.4) |
| Total | 12 (44.5) | 15 (55.5) | 27(100.0) | |
BP, biological prosthesis; MP, mechanical prosthesis.
Table 4
| Type | Frequency | Observations |
|---|---|---|
| Infections | 2 | Wound suppuration, secondary infection of chest wall |
| Hemorrhages | 2 | Hemopericardium needing surgical drainage |
| Conduction disturbances | 1 | Complete AV block, needing pacemaker placement |
| Thromboembolic event | 1 | Ischemic stroke |
| Others | 2 | Pneumopathy |
Discussion
We carried out this cross-sectional descriptive study at the DGH with the aim of reporting the disease profile, surgical uptake, and outcome of the first 3 years of the Cardiac surgery programme. The outcome of this North-South collaboration was successful. Most of the cases were rheumatic valvular heart disease and congenital heart disease. The surgical uptake was low.
A major limitation of this study is the small size. No case of coronary bypass graft was captured. This is however a less frequent disease condition, and the few cases needing surgery are treated abroad. We are in the pilot phase of this programme, which shows the potential of treating common disease conditions locally.
RHD is the most frequent acquired valvulopathy in low-income settings. The diagnosis is usually made late when significant valvular destructions have developed necessitating surgical intervention (5). Congenital heart diseases are also frequent, with most cases diagnosed late in life. Our findings are consistent with that reported by Ngatchou et al. who reported RHD in up to 72% of patients (4). This stresses the need to put in place effective primary and secondary preventive programmes of RHD in our setting, as the cost of surgery still remains high for most patients (2). All age groups can benefit from heart surgery locally with good outcomes. This is consistent with other reports from SSA, where patients as old as 85 years benefitted from heart surgery (6,7). Life expectancy in SSA is increasing, with a resultant double burden of RHD and degenerative heart disease that require surgery. There are differences on the burden and surgical uptake according to sex in the rare SSA literature. This stress the need to compile such data so as to have a better view (3,7,8).
Valve replacement was the most frequent surgical procedure in low-income settings. We attributed this to high prevalence of RHD in Africa (3,4). RHD is a chronic inflammatory condition involving the heart valves. Repairing such valves might be associated with subsequent surgery due to the progressive nature of the disease, thereby incurring an additional cost. However, most patients are seen at an advanced stage of the disease, with valve replacement surgery as the only option. The type of prosthesis implanted (mechanical or bioprosthesis) in our series depends on patient preference to an extent. Kingue et al. reported a high rate of bioprosthesis implantation due to the difficulties associated with managing anti-coagulants when mechanical valves are inserted in low-income settings (3). Open heart surgery was carried out in most series, probably due to the high rates of advanced valvular heart diseases and complex congenital heart diseases encountered (7). Trans-catheter closed heart surgery is not well developed in our setting.
The early surgical mortality rate varied across series, as low as 1.6% (7), and as high as 42.9% (6). This could be due to the choice of patients admitted into surgery. This however deserves a closer look. Two of our patients (7.4%) died in the early post-operative period due to acute ventricular failure. No other case of death has been recorded in our series in the long term. The quality of life was best in those operated for congenital heart disease in our series.
The rate of post-surgical infections also varied across series, as low as no complication (7), and as high as 18.1% (3). We do not have a clear explanation for this variation as this is multifactorial.
Due to the complexity of operated cases, these results of the first 3 years of the Cardiac surgery programme could be considered as good when compared to that reported in the literature (9-11).
Conclusions
The results of the pilot phase of cardiac surgery programme in Douala, Cameroon was successful. This was made possible by the close collaboration between the Cameroonian and Belgian teams. The continuity of the project requires the re-enforcement of technical platform, increase the human resource capacities, and subsidize surgery through a universal health coverage due to the low uptake encountered.
Acknowledgments
We thank Ahmadou Musa Jingi (MD, DES Internal Medicine) for critically reviewing the final manuscript.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2017.08.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This work was approved by the institutional review board of the Douala General Hospital (DGH) (Ref. No. 038AR/MINSANTE/HGD/DM/02/16). Informed consent was taken from all subjects.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Touze JE. Cardiovascular diseases and the epidemiological transition in tropical regions. Med Trop (Mars) 2007;67:541-2. [PubMed]
- Diarra MB, Ba HO, Sanogo KM, et al. The cost of evacuations for cardiovascular diseases and the needs for surgical and interventional treatment in Mali. Cardiol Trop 2006;32:66-8.
- Kingue S, Ngodjoum N, Muna W, et al. The Cameroon experience of Cardiac surgery: a report of 83 cases operated between 1985 – 1990. Cardiol Trop 1994;20:5-11.
- Ngatchou W, Lemogoum D, Ménanga AP, et al. Cardiac surgery in Cameroon. Results at one year of the pilot phase. Rev Med Brux 2011;32:14-7. [PubMed]
- Marijon E, Ou P, Celermajer DS, et al. Prevalence of rheumatic heart disease detected by echocardiographic screening. N Engl J Med 2007;357:470-6. [Crossref] [PubMed]
- Anyanwu CH, Ihenacho HN, Okoroma EO, et al. Initial experience in open heart surgery in Nigeria. Trop Cardiol 1982;8:123-7.
- Metras D, Coulibaly A, Ouattara K, et al. Cardiac surgery at the Institute of cardiology of Abidjan 1978-1983. Study of 728 surgical operations including 501 open heart. Cardiol Trop 1984;81-7.
- Moore AG. Rheumatic Heart Disease. In: Murphy JG, Lloyd MA. Editors. Mayo Clinic Cardiology, 3rd edition. Rochester: Mayo Clinic Scientific Press, 2007:549-54.
- Yangni Angate H, Ayegnon G, Meneas CH, et al. Open Heart Surgery in Chirurgie in Côte d’Ivoire. Twenty years of surgical experience. Ann Afr Chir Cardiovasc 2006;1:23-8.
- Kanga M, Yapobi Y, Tanauh Y, et al. Bioprosthesis Valvular Replacement in Africans less than 20 years. Our actual attitude. Médecine Afr Noire 1993;40:530-3.
- Brousse V, Imbert P, Mbaye P, et al. Evaluation of long-term outcome of Senegalese children sent abroad for cardiac surgery. Med Trop (Mars) 2003;63:506-12. [PubMed]
Cite this article as: Kamdem F, Ngatchou W, Hamadou B, Mboulley A, Luma H, Doualla MS, Lemogoum D, Germay O, Jansens JL, Origer P, Berre J, Dehon P, Alima MB, Dzudie A, Ngote H, Monkam Y, Mouliom S, Hentchoua R, Kana A, Coulibaly A, Belley Priso E, Kingue S. Cardiac surgery in sub-Saharan Africa: a report of 3-year experience at the Douala General Hospital. J Xiangya Med 2017;2:67.