
The historical evolution of the six-minute walk test as a measure of functional exercise capacity: a narrative review
Introduction
Functional capacity is the ability of a person to carry out daily activities of living such as walking, bathing or moving about, objectively quantified as the maximal oxygen consumption (VO2max) during a maximal-effort cardiopulmonary exercise test (CPET) (1,2). In the literature, the term “functional capacity” has often been interchangeably used with closely related, but sometimes different, terms such as “functional exercise capacity” (3), “working capacity”(4), “physical fitness” (4,5), “physical performance” (6), “cardiorespiratory performance” (6), “exercise tolerance” (7), “exercise capacity” (8), “cardiorespiratory fitness” (9,10), “functional status” (11,12), “walking capacity” (13), “aerobic fitness” (14), “aerobic power” (14), “ambulatory endurance” (15) and “cardiovascular fitness” (14).
The concept of evaluating a patient’s functional capacity arose from a progressive understanding of the biopsychosocial model of health, in which diseases (or injuries) result, not only in derangements of normal bodily functions or structures, but also in limitation of the person’s day-to-day activities and restriction of the person’s participation in societal responsibilities (Figure 1) (16). Thus, the optimal care of such a person requires the measurement, evaluation and amelioration of these disease-associated activity limitation and participation restriction, in addition to the cure or amelioration of the underlying or primary physiological derangements (17).
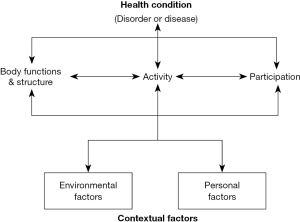
The gold-standard test for the objective quantification of functional capacity—CPET—is a highly sophisticated laboratory-based test that requires special costly equipment and specially-trained personnel. Consequently, it is not readily accessible to patients especially in primary care, necessitating need for simpler but similarly valid and reliable field measures of functional capacity (4,17,18). Currently, the most widely studied valid and reliable field measure of functional capacity is the six-minute walk test (6MWT)—a simpler and cheaper test that quantifies functional capacity using the distance walked in six minutes [the six-minute walk distance (6MWD)] at a self-selected pace on a hard surface such a hospital corridor (1,2,19,20). Whereas the VO2max measured during a CPET evaluates the physiological derangement domain of health, the 6MWD measured during a 6MWT predominantly evaluates the activity limitation domain (17). Hence, the 6MWT complements the CPET in the functional evaluation of patients but, occasionally, it may serve as an alternative where CPET is unavailable (21). Despite some limitations, the usefulness of the 6MWT has been demonstrated in numerous chronic adult and paediatric disorders, spanning the cardiopulmonary, musculoskeletal, neuromuscular, metabolic, endocrine and haematologic systems (1,22,23).
Although there exists a large and growing body of literature on various aspects of the 6MWT [for example, its measurement properties (2,15,22-29), clinical utility and methodology (1,15,19,27,30-33) and reference standards (20,34-40)], there has been limited attempts to present, in one paper, a detailed chronological record of important milestones in its evolution from pre-existing measures of functional capacity to its current status as the most widely used measure of functional capacity (41-44). Such a paper will provide a ‘one-stop shop’ and up-to-date reference of historical aspects of the test as well as key resources such as systematic reviews/meta-analyses of various aspects of the test for the benefit of clinical practitioners and researchers.
Methods & results
As part of a prior literature search for a project on the 6MWT of healthy Nigerian children (38), we conducted broad, unrestricted searches for papers related to 6MWT on multiple databases and search engines (PubMed, Google Scholar, Scopus, SciELO, Google, Yahoo and Bing) at various times from 2013 to August, 2018. The search terms used included “six-minute walk test” and its variations such as “6MWT”, “6-minute walk test”, “six-minute walking test” and also various forms of “functional capacity” such as “functional exercise capacity” or “exercise capacity”. The term “history” was also included to search for specific articles that may have chronicled the historical aspects of the 6MWT.
There was no restriction on the papers selected in terms of date of publication, type of work (full-text journal article, theses, conference abstracts or posters), geographical origin of work, subjects’ age ranges or language of publication. English translations of non-English articles were requested from the authors and when this was not available or feasible, translation was done with the aid of Google Translate. With respect to this narrative review, no strict quality criteria were applied on the articles but only articles with information relevant to the construction of the chronological development of the 6MWT from pre-existing measures of functional capacity, its utilisation as a primary measure of functional capacity in disease and health and development of reference standards for its clinical use were included.
References of selected articles were further searched for additional relevant articles. Retrieved articles were stored in a database until needed. English translation to one of the selected articles originally written in Arabic was provided by the authors (45) while three other articles (46-48) in Spanish were translated to English using Google Translate.
Discussion
From the laboratory to the “field”
The 20th century witnessed the steady development of the laboratory-based CPET and the elaboration of sophisticated gas-measuring equipment (6,49,50). Following the invention of the cycle ergometer in the early 1920s, the maximal oxygen uptake (VO2max)—defined as the maximal amount of oxygen an exercising individual consumes during maximal CPET-became recognised as the gold-standard measure of functional capacity (5,6,10,50-52). Researchers such as Taylor and colleagues (6) and Mitchell and co-workers (51) published earlier protocols for the standardised performance of CPET. However, there were concerns that the CPET, apart from requiring sophisticated equipment, was relatively time-consuming as only one person could be tested at a time. Thus, the original search for field-based measures of functional capacity arose out of the need for valid and reliable tests that could be administered to a large number of healthy individuals (military personnel) at the same time using relatively simple equipment (4,18,53).
The most cited earliest documented attempt at this was by Balke (4) in 1963. The author quantified the amount of oxygen consumed by a group of exercising subjects at increasing velocities while running on a treadmill in order to determine the VO2max. Thereafter, the subjects ran on a 1-mile long course on a field for varying durations of time at the fastest possible pace and the velocities achieved were calculated. The author observed that oxygen consumption (VO2) attained during the 12–20th minute of running was similar to VO2max attained on a treadmill. It was thus concluded that a 15-minute run test (15MRT) was equivalent to a maximal-effort CPET. Subsequently, the test was applied in the evaluation of aviation staff, obese subjects and sick persons.
In 1968, Cooper (18) sought to modify Balke’s 15MRT by studying 115 Airforce men who ran for 12 minutes at the fastest pace [12-minute run test (12MRT)]. The oxygen consumption calculated from the run test had an excellent correlation (r=0.897) with the VO2max attained on a treadmill and thus the author concluded that the 12MRT was similar in performance to Balke’s 15MRT. Thereafter, Cooper’s 12MRT has been extensively used in the functional evaluation of military personnel and athletes. Cooper (54) subsequently published age- and sex-based nomograms for estimating VO2max from distances attained during a 12MRT.
McGavin and colleagues (7), in 1976, argued that walking mimics daily activities better than running on a treadmill or cycling on an ergometer; hence, distances attained during a walk test would reflect daily functional impairments better than cycling or running. This argument was consequent to earlier studies such as that of Spiro and co-workers (55) who showed that maximal level of exertion (as may occur with running) was not required to assess functional capacity. Thus, McGavin et al. (7) modified Cooper’s 12MRT to a 12-minute walk test (12MWT) and applied it on subjects with chronic obstructive pulmonary disease (COPD) along a hospital’s indoor corridor. The 12-minute walk distance (12MWD) attained by the subjects correlated significantly with VO2max attained during a CPET.
Similarly, in 1977, Mungall and Hainsworth (9) demonstrated the reproducibility of the 12MWT as a measure of functional capacity. These researchers also observed that the 12MWD was a better measure of the impairment of daily functioning compared to forced expiratory volume in one second (FEV1). McGavin et al. (56) also later noted that the 12MWT was a better and more objective measure of functional capacity compared to subject-reported questionnaires. Thereafter, McGavin’s 12MWT became common as an objective measure of functional capacity, including in clinical trials of adults with chronic lung diseases (56-62).
6MWT in adult subjects
McGavin’s 12MWT continued as a commonly used field-based measure of functional capacity until in 1982 when Butland and co-workers (63) considered the 12MWT to be “both time consuming for the investigator and exhausting for the patient”. This group thus tested the hypothesis that walk tests of shorter duration [two-minute walk test (2MWT) and 6MWT] would have similar performances to the 12MWT in the measurement of functional capacity. It was observed that the subjects attained the highest walk velocity within the first two minutes after which the distances attained at subsequent two-minute intervals stabilized. The correlations among the three tests were excellent (6MWD vs. 12MWD, r=0.955; 2MWD vs. 12MWD, r=0.864; and 6MWD vs. 2MWD, r=0.892; n=30) with the mean 12MWD being twice the mean 6MWD of the subjects and the mean 6MWD approximately thrice the mean 2MWD. The authors thus concluded that the 6MWT was a “sensible compromise” between a rather too-long 12MWT and a relatively poorly-discriminatory 2MWT.
Two years after the ‘birth’ of Butland’s 6MWT, Guyatt et al. (8) reported that the 6MWT, compared to the 2MWT, had better ability to detect clinically meaningful change in functional capacity. Thereafter, the 6MWT increasingly became the most used field test for the measurement of functional capacity in adults with chronic diseases (23). It was used mainly in adults with chronic airway diseases until in 1985 when Guyatt et al. (11,64,65) reported that the 6MWT correlated significantly with CPET and the New York Heart Association (NYHA) functional classification scores in adults with chronic heart failure. Similarly, in 1986, Lipkin et al. (66) found the 6MWT useful and less exerting than CPET in the measurement of the functional capacity of adults with chronic heart failure. Subsequently, its utility was extended beyond the cardiopulmonary domain to individuals with metabolic, haematologic, neuromuscular, rheumatologic, psychiatric, renal and chronic infectious disorders (1,20,23,24,30,67-69).
6MWT in paediatric subjects
The earliest reports of the use of 6MWT in paediatric subjects were in two separate studies of Dutch and American children by Gulmans et al. (70) and Nixon et al. (71), respectively, both in 1996. The authors demonstrated the validity and reliability of the 6MWT as a measure of the functional capacity of children with cystic fibrosis and end-stage cardiopulmonary disorders. Thereafter, the 6MWT was tested and utilised in other chronic disorders of childhood such as congenital heart diseases, end-stage renal disease, obesity, cerebral palsy and HIV infection (22,72-74).
Standardisation of the 6MWT
In 1984, Guyatt et al. (8) in a randomised interventional study of 43 adults with chronic cardiopulmonary disorders, observed that differential encouragements administered during a 6MWT significantly affected the distance achieved and thus recommended its standardisation. However, a comprehensive standardisation of the 6MWT was not available until in 2002 when the Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories of the American Thoracic Society (ATS) (1) published the first standard guidelines in order to harmonise its clinical application and enhance international comparison across studies. This statement provided guidelines on patient selection, equipment, indications and contraindications, standardised minute-by-minute encouragements and other aspects of the test in adult populations.
In two subsequent, long-overdue, reviews of the 2002 ATS guidelines, the ATS in conjunction with the European Respiratory Society (ERS) provided updates on the measurement properties (2) and “standard operating procedures” (30) of the 6MWT. The updates, in contrast to the 2002 guidelines, were more emphatic on the need for repeat testing when used for post-interventional evaluation in order to account for “learning effect”. In 2015, the Polish Respiratory Society also issued consensus guidelines on the 6MWT (19).
Reference standards for the 6MWT in adults
Following the establishment of the validity and reliability of the 6MWT as a measure of functional capacity, the need for reference standards (reference values with or without predictive regression equations) became obvious in order to guide clinical interpretation of the test. The first reference standards and equations in adults were published by Enright and Sherill (75) in 1988 in a study of 290 healthy adults in USA. The 6MWD was independently predicted by height, weight, body mass index (BMI), age and sex. Thereafter, Troosters et al. (76) in 1999 and Gibbons et al. (77) in 2001 published reference equations derived from healthy Belgian and Canadian adults, respectively.
These three studies were published before the 2002 ATS guidelines and so were characterized by wide variability in test protocols including course lengths and encouragements. Subsequent to the publication of the 2002 ATS guidelines, there was widespread development of reference standards and equations from various ethno-geographic regions of the world (20,39,78-81). Salbach et al. (80) in 2014 published a systematic review conducted on 20 studies that published prediction reference equations emanating from American, European, Asian and African adult populations. Additional equations that have been published after this Salbach’s review are shown in Table 1.
Table 1
| Author (country, year) | Prediction reference equation(s) |
|---|---|
| Rao et al. (Pakistan, 2011) (82) | 6MWD =164.08+ (78.06× G) − (1.90× A) + (195× H); R2 =0.330 |
| Ajiboye et al. (Nigeria, 2014) (39) | 6MWD = (419.83× H) – (1.02× A) – (1.03× W) –79.02; R2 =0.303 |
| Ngai et al. (China, 2014) (83) | 6MWD =722.35– (5.11× A) + (2.19× %predHRmax) – (41.31× G); R2 =0.650 |
| Kim et al. (Korea, 2014) (84) | 6MWD =105.7 + (299× H); R2 =0.205 |
| Ramanathan & Chandrasekaran (India, 2014) (85) | M: 6MWD =561.02− (2.51× A) + (1.51× W) − (5.50× H); R2 =0.288 |
| F: 6MWD =30.325− (0.81× A) − (2.07× W) + (424× H); R2 =0.272 | |
| Beekman et al. (Netherlands, 2014) (86) | M: 6MWD =1073− (6.03× A) − (5.79× BMI) + (1.86× HRdiff); R2 =0.62 |
| F: 6MWD =878− (3.60× A) − (6.42× BMI) + (1.95× HRdiff); R2 =0.71 | |
| Tveter et al. (Norway, 2014) (87) | 6MWD = −224.28 + (591× H) − (1.61× W); R2 =0.370 |
| Nusdwinuringtyas et al. (Indonesia, 2014) (88) | 6MWD =586.25+ (0.62× W) – (26.50× H) – (63.34× G) + (0.117× A); R2 =0.367 |
| Bourahli et al. (Algeria, 2015) (89) | 6MWD =800.05 + (64.71× G) + (10.23× BMI) + (1.63× A) + (2.05× W); R2 =0.587 |
| Fernandes et al. (India, 2016) (90) | 6MWD =553.29+ (−2.11× A) + (45.32× G); R2 =0.307 |
| Zou et al. (China, 2017) (91) | F: 6MWD =233.99− (1.82× A) + (263× H); R2 =0.34 |
| M: 6MWD =141.33– (1.04× A) + (304× H); R2 =0.28 | |
| Vaish et al. (India, 2017) (92) | F: 6MWD =856.55– (16.08× A); R2 =0.350 |
| M: 6MWD =681.97– (19.99× A) + (206× H); R2 =0.27 | |
| Padmavathy et al. (Malaysia, 2018) (93) | F: 6MWD =441.08+ (52.90× H) + (0.646× W) + (2.601× CE) |
| M: 6MWD =60.06+ (236.70× H) + (0.780× W) + (18.04× CE) | |
| Shrestha & Srivastava (Nepal, 2015) (94) | 6MWD =395– (1.5× A) + (2.47× W) – (35.89× G) |
| Alqahtani (US African-Americans, 2017) (78) | 6MWD =8.00+ (78.39× G) + (2.02× PostHR) + (203× H); R2 =0.58 |
*, not included in previous systematic reviews (80). 6MWD, six-minute walk distance in meters; M, men; F, women; G, gender, where M =1, F =0, except for the Indonesian study where F =1 and M =0; A, age in years; H, height in meters; W, weight in kg; HR, heart rate in beats/min; HRdiff, heart rate difference; R2, coefficient of determination; PostHR, post-exercise heart rate; %predHRmax, percentage predicted maximal heart rate; CE, chest expansion in cm.
6MWT reference standards in paediatric age groups
The publication of reference standards for the 6MWT in children lagged behind that of the adult population, arguably due to concerns about safety and validity. Also, because of lack of paediatric-specific guidelines on the 6MWT (till date), studies in both healthy and sick paediatric subjects have extrapolated the existing adult guidelines to children, frequently with methodological modifications such as use of shorter course lengths, incentive devices or “safety chasers” (22,34-36,38,95-98).
The first published reference standards (mean 6MWD without equations) from healthy children was from a study of Chilean subjects by Escobar et al. (47) in 2001. Later in 2007, Li et al. (99) published the first predictive regression equations for the 6MWD of healthy Chinese children and adolescents (99). Subsequently, reference standards (with or without equations) were published from healthy European, American, Asian and African paediatric populations. Most of these reference standards and equations have been summarized in three separate systematic reviews by Cacau et al. (36), Mylius et al. (34) and Rodríguez-Núñez et al. (40). Reference equations that were not included or that were published after publication of these reviews are presented in Table 2 (34,36,38).
Table 2
| Authors (country, year) | Prediction reference equation(s) |
|---|---|
| Acosta García et al. (Venezuela, 2012) (48) | 6MWD =444.68+ (27.88× A); R2 =0.46 |
| Ubuane (Nigeria, 2017) (38) | 6MWD =337.0+ (15.4× A) + (19.5× G) + (1.6× HRdiff) + (1.2× SBPdiff); R2 =0.282 |
| Vandoni et al. (Italy, 2018) (100) | 6MWD = −160.16+ (93.35× A) − (4.05× A*2) + (7.34× G) + (2.12× W) − (250× H) |
| Jalili and Nazem (Iran, 2017) (45) | M: 6MWD =644.83+ (18.52× A) – (8.24× BMI); R2 =0.627 |
| de Assis Pereira Cacau et al. (Brazil, 2018) (35) | M: 6MWD = (16.86× A) + (1.89× HRdiff) – (0.80× W) + (336.91× R1) + (360.91× R2) F: 6MWD = (13.54× A) + (1.62× HRdiff) – (1.28× W) + (352.33× R1) + (394.81× R2) |
*, not included in previous systematic reviews (34,36,40). 6MWD, six-minute walk distance in meters; M, boys; F, girls; G, gender, where M =1, F =0; A, age in years; H, height in meters; W, weight in kg; HR, heart rate in beats/min; HRdiff, heart rate difference; SBPdiff, systolic blood pressure difference; R2, coefficient of determination; R1 & R2, geographical regions of residence in Brazil-North vs. South.
In both adult and paediatric studies, the need for reference values and equations specific to each ethno-geographic region have been informed/justified by an observation of wide variation in the reference values (34,36,40,79,80). Thus, independent of differences in test methodologies and other influencing variables such as anthropometrics characteristics, race and ethnicity significantly influence subjects’ performance on the 6MWT (34,36,40,101).
Novel approaches and innovations
The last decade has witnessed interesting innovations aimed at improving the efficiency of administering the 6MWT, as well as reducing the manpower required to conduct the test. For example, Du and colleagues (27,102) conceptualised the use of the 6MWT as a home-based “self-administered” measure of the functional capacity of community-dwelling patients with chronic heart failure (home-heart-walk test). This aimed to provide ambulatory patients with chronic heart disease with a self-monitoring tool (akin to self-monitoring with glucometer in diabetes care or hand-held spirometers in chronic lung diseases) that could help in the early detection and tracking of changes in their functional capacity while at home (27).
With the advent and widespread availability of smart-phones, administration of the 6MWT has been further enhanced with the development and validation of smart-phone applications that combine the functions of lap counter, stopwatch and calculator into a single application for use during a 6MWT at home or in clinic settings (103). Furthermore, applications that not only do the aforementioned but also use phone-based sensors such as gyroscopes to auto-derive the 6MWD (without counting the number of laps) and transmit the data remotely to clinicians have been developed (104). Thus, the 6MWT has come to stay as a relevant measure of functional capacity of patients with chronic diseases.
Conclusions
From its first documented use in the early 1980s, the 6MWT has become the most commonly used valid and reliable field-based objective measure of functional capacity in both adult and paediatric populations (23). A large and growing body of data exists on its development, utility, measurement properties and reference equations across various ethno-geographic populations. Apart from chronicling its evolution over the years, this review has highlighted prominent persons or groups who made contributions to its development. There is however need for paediatric-specific guidelines for use in children and adolescents. Also, reference equations are needed in children from other ethnic groups such as North American and other sub-Saharan African regions.
Acknowledgements
We express gratitude to authors who provided translations or full texts of their works on request.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2018.11.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111-7. Erratum in: Erratum: ATS Statement: Guidelines for the Six-Minute Walk Test [Am J Respir Crit Care Med 2016]. [Crossref] [PubMed]
- Singh SJ, Puhan MA, Andrianopoulos V, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Respir J 2014;44:1447-78. [Crossref] [PubMed]
- The Criteria Committee of the New York Heart Association. Functional exercise capacity and objective assessment. 9th edition. Boston, MA: Little, Brown and Co., 1964.
- Balke B. A simple field test for the assessment of physical fitness. REP 63-6. Rep Civ Aeromed Res Inst US 1963:1-8.
- Robinson S. Experimental studies of physical fitness in relation to age. Arbeitsphysiologie 1938;10:251-323.
- Taylor HL, Buskirk E, Henschel A. Maximal Oxygen Intake as an Objective Measure of Cardio-Respiratory Performance. J Appl Physiol 1955;8:73-80. [Crossref] [PubMed]
- McGavin CR, Gupta S, McHardy G. Twelve-minute walking chronic bronchitis for assessing disability. Br Med J 1976;1:822-3. [Crossref] [PubMed]
- Guyatt GH, Pugsley S, Sullivan MJ, et al. Effect of encouragement on walking test performance. Thorax 1984;39:818-22. [Crossref] [PubMed]
- Mungall IP, Hainsworth R. Assessment of respiratory function in patients with chronic obstructive airways disease. Thorax 1979;34:254-8. [Crossref] [PubMed]
- Shephard RJ, Allen C, Benade AJ, et al. The maximum oxygen intake. An international reference standard of cardiorespiratory fitness. Bull World Health Organ 1968;38:757-64. [PubMed]
- Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: A new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J 1985;132:919-23. [PubMed]
- World Health Organization. The International Classification of Functioning, Disability and Health 2001;18:237. Available online: http://www.who.int/classifications/icf/en/. Assessed 2015-08-23.
- Takeuchi Y, Katsuno M, Banno H, et al. Walking capacity evaluated by the 6-minute walk test in spinal and bulbar muscular atrophy. Muscle Nerve 2008;38:964-71. [Crossref] [PubMed]
- Takken T, Bongers BC, Van Brussel M, et al. Cardiopulmonary Exercise Testing in Pediatrics. Ann Am Thorac Soc 2017;14:S123-8. [Crossref] [PubMed]
- Steffen TM, Nelson RE. Measurement of Ambulatory Endurance in Adults. Top Geriatr Rehabil 2012;28:39-50. [Crossref]
- World Health Organization. Towards a Common Language for Functioning, Disability and Health: ICF. The International Classification of Functioning, Disability and Health 2002;1149:1-22. Available online: http://www.who.int/classifications/icf/training/icfbeginnersguide.pdf
- Bui KL, Nyberg A, Maltais F, et al. Functional Tests in Chronic Obstructive Pulmonary Disease, Part 1: Clinical Relevance and Links to the International Classification of Functioning, Disability, and Health. Ann Am Thorac Soc 2017;14:778-84. [Crossref] [PubMed]
- Cooper KH. A Means of Assessing Maximal Oxygen Intake. JAMA 1968;203:201-4. [Crossref] [PubMed]
- Przybyłowski T, Tomalak W, Siergiejko Z, et al. Polish Respiratory Society guidelines for the methodology and interpretation of the 6 minute walk test (6MWT). Pneumonol Alergol Pol 2015;83:283-97. [Crossref] [PubMed]
- Andrianopoulos V, Holland AE, Singh SJ, et al. Six-minute walk distance in patients with chronic obstructive pulmonary disease: Which reference equations should we use? Chron Respir Dis 2015;12:111-9. [Crossref] [PubMed]
- Rostagno C, Gensini GF. Six minute walk test: a simple and useful test to evaluate functional capacity in patients with heart failure. Intern Emerg Med 2008;3:205-12. [Crossref] [PubMed]
- Bartels B, de Groot JF, Terwee CB. The six-minute walk test in chronic pediatric conditions: a systematic review of measurement properties. Phys Ther 2013;93:529-41. [Crossref] [PubMed]
- Solway S, Brooks D, Lacasse Y, et al. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest 2001;119:256-70. [Crossref] [PubMed]
- Vickers RR. Walk tests as indicators of aerobic capacity. California: Naval Health Research Center, 2002.
- Bui KL, Nyberg A, Maltais F, et al. Functional Tests in Chronic Obstructive Pulmonary Disease, Part 2: Measurement Properties. Ann Am Thorac Soc 2017;14:785-94. [Crossref] [PubMed]
- Shoemaker MJ, Curtis AB, Vangsnes E, et al. Triangulating Clinically Meaningful Change in the Six-minute Walk Test in Individuals with Chronic Heart Failure: A Systematic Review. Cardiopulm Phys Ther J 2012;23:5-15. [Crossref] [PubMed]
- Du H, Newton PJ, Salamonson Y, et al. A review of the six-minute walk test: Its implication as a self-administered assessment tool. Eur J Cardiovasc Nurs 2009;8:2-8. [Crossref] [PubMed]
- Bellet RN, Adams L, Morris NR. The 6-minute walk test in outpatient cardiac rehabilitation: validity, reliability and responsiveness-a systematic review. Physiotherapy 2012;98:277-86. [Crossref] [PubMed]
- Schrover R, Evans K, Giugliani R, et al. Minimal clinically important difference for the 6-min walk test: literature review and application to Morquio A syndrome. Orphanet J Rare Dis 2017;12:78. [Crossref] [PubMed]
- Holland AE, Spruit MA, Troosters T, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J 2014;44:1428-46. [Crossref] [PubMed]
- Enright PL. The Six-Minute Walk Test. Respir Care 2003;48:783-5. [PubMed]
- Faggiano P, D’Aloia A, Gualeni A, et al. The 6 minute walking test in chronic heart failure: indications, interpretation and limitations from a review of the literature. Eur J Heart Fail 2004;6:687-91. [Crossref] [PubMed]
- Dunn A, Marsden DL, Nugent E, et al. Protocol variations and six-minute walk test performance in stroke survivors: a systematic review with meta-analysis. Stroke Res Treat 2015;2015:484813. [Crossref] [PubMed]
- Mylius CF, Paap D, Takken T. Reference value for the 6-minute walk test in children and adolescents: a systematic review. Expert Rev Respir Med 2016;10:1335-52. [Crossref] [PubMed]
- de Assis Pereira Cacau L, Carvalho VO, Dos Santos Pin A, et al. Reference Values for the 6-min Walk Distance in Healthy Children Age 7 to 12 Years in Brazil: Main Results of the TC6minBrasil Multi-Center Study. Respir Care 2018;63:339-46. [Crossref] [PubMed]
- Cacau LA, de Santana-Filho VJ, Maynard LG, et al. Reference Values for the Six-Minute Walk Test in Healthy Children and Adolescents: A Systematic Review. Braz J Cardiovasc Surg 2016;31:381-8. [PubMed]
- Bohannon RW. Six-Minute Walk Test: A Meta-Analysis of Data From Apparently Healthy Elders. Top Geriatr Rehabil 2007;23:155-60. [Crossref]
- Ubuane PO. Predictive reference equation for the six-minute walk distance of apparently healthy primary school pupils in Ikeja, Lagos State. Faculty of Paediatrics, West African College of Physicians, 2017.
- Ajiboye OA, Anigbogu CN, Ajuluchukwu JN, et al. Prediction equations for 6-minute walk distance in apparently healthy Nigerians. Hong Kong Physiother J 2014;32:65-72. [Crossref]
- Rodríguez-Núñez I, Mondaca F, Casas B, et al. Normal values of 6-minute walk test in healthy children and adolescents: A systematic review and meta-analysis. Rev Chil Pediatr 2018;89:128-36. [PubMed]
- Vuckovic KM, Fink AM. The 6-Min Walk Test: Is It an Effective Method for Evaluating Heart Failure Therapies? Biol Res Nurs 2012;14:147-59. [Crossref] [PubMed]
- Grinnell D. The Historical and Clinical Significance of the 6- Minute Walk Test 1960. Available online: http://www.slideshare.net/dgrinnell/the-historical-and-clinical-significance-of-the-6-minute-walk-test?from_action=save (accessed July 31, 2015).
- Zieliński J. Six minute walking test: an old tool with new applications. Multidiscip Respir Med 2010;5:241-2. [Crossref] [PubMed]
- Venkatesh N, Thanikachalam S, Satyanarayana M, et al. Six minute walk test: a literary review. Sri Ramachandra J Med 2011;4:30-4.
- Jalili M, Nazem F. Design and Cross-Validation of Six-Minute Walk Test (6MWT) Prediction Equation in Iranian healthy Males Aged 7 to 16 Years. J Ergon 2017;5:17-25. [Crossref]
- Gatica D, Puppo H, Villarroel G, et al. Reference values for the 6-minutes walking test in healthy Chilean children (article in Spanish). Rev Med Chile 2012;140:1014-21. [Crossref] [PubMed]
- Escobar M, López A, Veliz C, et al. Six minute walking test in healthy Chilean children (article in Spanish). Kinesiologia 2001;62:16-20.
- Acosta García EJ, Rodriguez LS, Barón MA, et al. Six-minute walk test in school children (article in Spanish). Salus 2012;16:25-9.
- Astrand PO, Saltin B. Maximal oxygen uptake and heart rate in various types of muscular activity. J Appl Physiol 1961;16:977-81. [Crossref] [PubMed]
- Seiler S. A Brief History of Endurance Testing in Athletes. Sportscience 2011;15:40-6.
- Mitchell JH, Sproule BJ, Chapman CB. The physiological meaning of the maximal oxygen intake test. J Clin Invest 1958;37:538-47. [Crossref] [PubMed]
- Hill AV. Muscular activity. Oxford, England: Bailliere, 1926.
- Mackenzie B. Cooper Test - 12 minute run to assess your VO2max. Www 1997. Available online: http://www.brianmac.co.uk/gentest.htm (accessed August 12, 2015).
- Cooper KH. The new aerobics. Bantam Books, 1970.
- Spiro SG, Hahn HL, Edwards RH, et al. An analysis of the physiological strain of submaximal exercise in patients with chronic obstructive bronchitis. Thorax 1975;30:415-25. [Crossref] [PubMed]
- McGavin CR, Artvinli M, Nace H, et al. Dyspnoea, disability and distance walked: Comparison of estimates of exercise performance in respiratory disease. Int J Rehabil Res 1980;3:235-6. [Crossref] [PubMed]
- Cockcroft AE, Saunders MJ, Berry G. Randomised controlled trial of rehabilitation in chronic respiratory disability. Thorax 1981;36:200-3. [Crossref] [PubMed]
- Calverley PM, Leggett RJ, Flenley DC. Carbon monoxide and exercise tolerance in chronic bronchitis and emphysema. Br Med J (Clin Res Ed) 1981;283:878-80. [Crossref] [PubMed]
- Butland RJ, Pang JA, Geddes DM. Carbimazole and exercise tolerance in chronic airflow obstruction. Thorax 1982;37:64-7. [Crossref] [PubMed]
- Leitch AG, Morgan A, Ellis DA, et al. Effect of oral salbutamol and slow-release aminophylline on exercise tolerance in chronic bronchitis. Thorax 1981;36:787-9. [Crossref] [PubMed]
- O’Reilly JF, Shaylor JM, Fromings KM, et al. The use of the 12 minute walking test in assessing the effect of oral steroid therapy in patients with chronic airways obstruction. Br J Dis Chest 1982;76:374-82. [Crossref] [PubMed]
- Williams AJ, Osman J, Skinner C. Effects of naftidrofuryl on breathlessness and exercise tolerance in chronic bronchitis. Thorax 1982;37:617-9. [Crossref] [PubMed]
- Butland RJA, Pang J, Gross ER, et al. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res Ed) 1982;284:1607-8. [Crossref] [PubMed]
- Guyatt GH, Thompson PJ, Berman LB, et al. How should we measure function in patients with chronic heart and lung disease? J Chronic Dis 1985;38:517-24. [Crossref] [PubMed]
- Guyatt GH, Townsend M, Keller J, et al. Measuring functional status in chronic lung disease: conclusions from a randomized control trial. Respir Med 1989;83:293-7. [Crossref] [PubMed]
- Lipkin DP, Scriven A J, Crake T, et al. Six minute walking test for assessing exercise capacity in chronic heart failure. Br Med J (Clin Res Ed) 1986;292:653-5. [Crossref] [PubMed]
- Adedoyin RA, Erhabor GE, Ojo OD, et al. Assessment of Cardiovascular Fitness of Patients with Pulmonary Tuberculosis Using Six Minute Walk Test. TAF Prev Med Bull 2010;9:99-106.
- Mbada CE, Onayemi O, Ogunmoyole Y, et al. Health-related quality of life and physical functioning in people living with HIV/AIDS: a case-control design. Health Qual Life Outcomes 2013;11:106. [Crossref] [PubMed]
- Ajiboye OA, Anigbogu CN, Ajuluchukwu JN, et al. Exercise training improves functional walking capacity and activity level of Nigerians with chronic biventricular heart failure. Hong Kong Physiother J 2015;33:42-9. [Crossref]
- Gulmans VA, van Veldhoven NH, de Meer K, et al. The six-minute walking test in children with cystic fibrosis: reliability and validity. Pediatr Pulmonol 1996;22:85-9. [Crossref] [PubMed]
- Nixon PA, Joswiak ML, Fricker FJ. A six-minute walk test for assessing exercise tolerance in severely ill children. J Pediatr 1996;129:362-6. [Crossref] [PubMed]
- Sims Sanyahumbi AE, Hosseinipour MC, Guffey D, et al. HIV-infected Children in Malawi Have Decreased Performance on the 6-minute Walk Test With Preserved Cardiac Mechanics Regardless of Antiretroviral Treatment Status. Pediatr Infect Dis J 2017;36:659-64. [Crossref] [PubMed]
- de Groot JF, Takken T. The six-minute walk test in paediatric populations. J Physiother 2011;57:128. [Crossref] [PubMed]
- Zuk M, Migdal A, Jagiellowicz-Kowalska D, et al. Six-Minute Walk Test in Evaluation of Children with Pulmonary Arterial Hypertension. Pediatr Cardiol 2017;38:754-61. [Crossref] [PubMed]
- Enright PL, Sherrill DL. Reference equations for the six-minute walk in healthy adults. Am J Respir Crit Care Med 1998;158:1384-7. [Crossref] [PubMed]
- Troosters T, Gosselink R, Decramer M. Six minute walking distance in healthy elderly subjects. Eur Respir J 1999;14:270-4. [Crossref] [PubMed]
- Gibbons WJ, Fruchter N, Sloan S, et al. Reference values for a multiple repetition 6-minute walk test in healthy adults older than 20 years. J Cardiopulm Rehabil 2001;21:87-93. [Crossref] [PubMed]
- Alqahtani M. Developing a prediction equation for the six-minute walk test in healthy African-American adults. Georgia State University, 2017.
- Casanova C, Celli BR, Barria P, et al. The 6-min walk distance in healthy subjects: reference standards from seven countries. Eur Respir J 2011;37:150-6. [Crossref] [PubMed]
- Salbach NM, Brien KKO, Brooks D, et al. Reference values for standardized tests of walking speed and distance : A systematic review. Gait Posture 2015;41:341-60. [Crossref] [PubMed]
- Mbada CE, Jaiyeola OA, Johnson OE, et al. Reference Values for Six Minute Walk Distance in Apparently Healthy Young Nigerian Adults (Age 18-35 Years). Int J Sport Sci 2015;5:19-26.
- Rao NA, Irfan M, Haque AS, et al. Six-Minute Walk Test Performance in Healthy adult Pakistani volunteers. J Coll Physicians Surg Pak 2013;23:720-5. [PubMed]
- Ngai SP, Jones AY, Jenkins SC. Regression equations to predict 6-minute walk distance in Chinese adults aged 55-85 years. Hong Kong Physiother J 2014;32:58-64. [Crossref]
- Kim AL, Kwon JC, Park I, et al. Reference equations for the six-minute walk distance in healthy Korean adults, aged 22-59 years. Tuberc Respir Dis (Seoul) 2014;76:269-75. [Crossref] [PubMed]
- Palaniappan Ramanathan R, Chandrasekaran B. Reference equations for 6-min walk test in healthy Indian subjects (25-80 years). Lung India 2014;31:35-8. [Crossref] [PubMed]
- Beekman E, Mesters I, Gosselink R, et al. The first reference equations for the 6-minute walk distance over a 10 m course. Thorax 2014;69:867-8. [Crossref] [PubMed]
- Tveter AT, Dagfinrud H, Moseng T, et al. Health-related physical fitness measures: Reference values and reference equations for use in clinical practice. Arch Phys Med Rehabil 2014;95:1366-73. [Crossref] [PubMed]
- Nusdwinuringtyas N. Reference equation for prediction of a total distance during six-minute walk test using Indonesian anthropometrics. Acta Med Indones 2014;46:90-6. [PubMed]
- Bourahli MK, Bougrida M, Martani M, et al. 6-Min walk-test data in healthy North-African subjects aged 16–40 years. Egypt J Chest Dis Tuberc 2016;65:349-60. [Crossref]
- Fernandes L, Mesquita AM, Vadala R, et al. Reference Equation for Six Minute Walk Test in Healthy Western India Population. J Clin Diagn Res 2016;10:CC01-4. [PubMed]
- Zou H, Zhu X, Zhang J, et al. Reference equations for the six-minute walk distance in the healthy Chinese population aged 18–59 years. PLoS One 2017;12:e0184669. [Crossref] [PubMed]
- Vaish H, Gupta S, Sharma S. Six Minute Walk Distance and Six Minute Walk Work in Young Adults Aged 18-25. Int J Pharm Med Res 2017;5:464-8.
- Padmavathy KM, Sankaran RS, Oncho TJ, et al. Six-Minute Walk Test: reference values for healthy young adults in Malaysia. Natl J Integr Res Med 2018;9:66-70.
- Shrestha SK, Srivastava B. Six minute walk distance and reference equations in normal healthy subjects of Nepal. Kathmandu Univ Med J 2015;13:97-101. (KUMJ). [Crossref] [PubMed]
- Geiger R, Strasak A, Treml B, et al. Six-minute walk test in children and adolescents. J Pediatr 2007;150:395-9. [Crossref] [PubMed]
- Goemans N, Klingels K, van den Hauwe M, et al. Six-minute walk test: reference values and prediction equation in healthy boys aged 5 to 12 years. PLoS One 2013;8:e84120. [Crossref] [PubMed]
- McDonald CM, Henricson EK, Han JJ, et al. The 6-minute walk test as a new outcome measure in Duchenne muscular dystrophy. Muscle Nerve 2010;41:500-10. [Crossref] [PubMed]
- Morales Mestre N, Audag N, Caty G, et al. Learning and Encouragement Effects on Six-Minute Walking Test in Children. J Pediatr 2018;198:98-103. [Crossref] [PubMed]
- Li AM, Yin J, Au JT, et al. Standard reference for the six-minute-walk test in healthy children aged 7 to 16 years. Am J Respir Crit Care Med 2007;176:174-80. [Crossref] [PubMed]
- Vandoni M, Correale L, Puci MV, et al. Six minute walk distance and reference values in healthy Italian children: A cross-sectional study. PLoS One 2018;13:e0205792. [Crossref] [PubMed]
- Dourado VZ. Reference Equations for the 6-Minute Walk Test in Healthy Individuals. Arq Bras Cardiol 2011;96:128-38. [Crossref] [PubMed]
- Du H, Davidson PM, Everett B, et al. Assessment of a Self-administered Adapted 6-Minute Walk Test. J Cardiopulm Rehabil Prev 2010;30:116-20. [Crossref] [PubMed]
- Brooks GC, Vittinghoff E, Iyer S, et al. Accuracy and usability of a self-administered 6-Minute Walk Test smartphone application. Circ Heart Fail 2015;8:905-13. [Crossref] [PubMed]
- Capela NA, Lemaire ED, Baddour N. Novel algorithm for a smartphone-based 6-minute walk test application: algorithm, application development, and evaluation. J Neuroeng Rehabil 2015;12:19. [Crossref] [PubMed]
Cite this article as: Ubuane PO, Animasahun BA, Ajiboye OA, Kayode-Awe MO, Ajayi OA, Njokanma FO. The historical evolution of the six-minute walk test as a measure of functional exercise capacity: a narrative review. J Xiangya Med 2018;3:40.


