Young lady presented with sudden loss of vision
Clinical case presentation
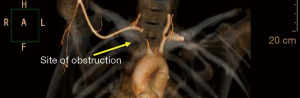
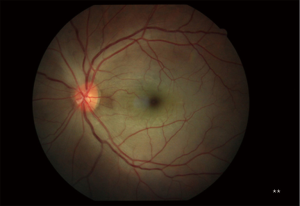
A 23-year-old female presented with a 3-month history of acute loss of vision in the right eye and 1 month history of loss of vision in the left eye. There was an associated severe retro-orbital headache. There was no history of vomiting, fever, skin rash, oral ulcers. No other co-morbidities or significant family history was present. On examination, mentation was found to be intact. Right upper limb pulse was absent and blood pressure was not recordable in that arm. Temperature was normal and no apparent signs of compartment syndrome or forearm ischemia were present. Bilateral carotid pulse was absent. Left upper limb blood pressure was 110/70 mmHg, Pupils were dilated and not reactive to light. Complete hemogram and biochemical investigations including a metabolic profile were normal. ECG, chest X-ray, and 2D Echocardiography were unremarkable. Her initial diagnosis was central retinal artery occlusion (CRAO) for which she underwent laser treatment without any improvement in her vision and was subsequently transferred to a larger tertiary referral centre. Contrast enhanced MRI brain was done which on T2/FLAIR sequences showed hyperintensity at bilateral Centrum semiovale along internal watershed zone and at the left paraventricular deep white matter, suggestive of ischemic change. Left vitreous chamber on T2/FLAIR sequences showed similar hyperintensity. Orbital ultrasonography (o-USG) correlation revealed features suggestive of retinal detachment. Doppler ultrasonography screening of the carotid artery revealed occlusive disease and therefore the patient was underwent evaluation by a neurologist. Takayasu arteritis was then diagnosed and revascularization of the obstructed vessels was considered. CT right upper limb and angiogram, revealed 50–60% proximal innominate artery luminal compromise, 90% distal innominate artery luminal compromise, 90% proximal right common carotid artery luminal compromised with circumferential mural thickening of the left common carotid artery involving proximal 50 mm. The detailed angiogram is shown in Figure 1. Fundus examination at presentation is shown in Figure 2.
The patient underwent successful PTA with a stent to right carotid and right subclavian artery. A 7.0×80 mm absolute pro self-expanding stent was used for this purpose after pre-dilation. Post-dilatation was subsequently performed shown in Figure 3. On table, the patient demonstrated improvement in her vision. The patient was initially started on pulse steroid therapy, each pulse cycle consisted of 3 days of IV methylprednisolone 1 g/day, Followed by oral corticosteroids 1 mg/kg/day and for systemic immunosuppression was continued on oral methotrexate 20 mg/week which aided in the recovery and suppression of disease. Interventional therapy for ocular Takayasu especially in the form of Central retinal artery occlusion (CRAO) include Vitrectomy/Nd:YAG laser.

Discussion
Takayasu arteritis disease is an uncommon inflammatory arteritis predominantly affecting the aorta and its branches (1). Uyama and Asayama broadly classified the ocular manifestations into three types (2), type 1 comprised of the ischemic ocular manifestations of Takayasu arteritis, termed as Takayasu Retinopathy which has been further classified into four stages. Stage one is characterized by the distention of veins, stage two consists of microaneurysm formation, the occurrence of arteriovenous anastomoses indicates stage three and complications like retinal ischemia, neovascularization, rubeosis iridis and vitreous hemorrhage occurs in stage four. The variability of ischemic changes in Takayasu arteritis probably depends upon the involvement of the carotid arteries which are occluded, and the duration and rate of ocular vascular insufficiency, in addition to the development of collateral blood supply. Ocular presentation of Takayasu arteritis is reported to vary between 8.1% and 68% of the patients (3). The ocular findings of the disease are related to carotid artery obliteration which leads to hypoperfusion of all the eye structures. Reduced blood flow in the carotid arteries causes Takayasu’s retinopathy which is related Takayasu arteritis the chronic ischemia and occurs in the late phase of the disease (4). Retinal vessel involvement, branch retinal artery occlusion, central retinal artery occlusion (CRAO), and branch retinal vein occlusion were demonstrated (5). Classical ophthalmological presentations are due to hypotension or hypertensive retinopathy. The ocular manifestation in the disease commonly results from the ocular hypotension secondary to occlusion of the arteries. The variable ocular presentations of Takayasu arteritis depend on the anatomy of the carotid artery occluded, duration, rate of vascular insufficiency and development of collateral blood supply (6). Revascularization-percutaneous transluminal angioplasty or bypass grafts may be considered in late cases when irreversible arterial stenosis has occurred and when significant ischemic symptoms are present (7). Percutaneous transluminal angioplasty is preferable when the stenosis is amenable to catheter based therapy. Percutaneous endovascular techniques provide a vista for prevention of irreversible neurological damage in the setting of impeding deficit. These techniques help in the immediate relief of occlusive disease. They provide the patient and physician with a means to temporize disease manifestations while systemic manifestations and disease progression is retarded by immunosuppressive therapy (8).
Conclusion
Although retinal artery involvement is a very rare presentation in Takayasu arteritis, it is important to consider Takayasu arteritis particularly in young patients with retinal artery occlusion. Early revascularization may perhaps limit vision loss.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2019.02.04). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chun YS, Park SJ, Park IK, et al. The clinical and ocular manifestations of Takayasu arteritis. Retina 2001;21:132-40. [Crossref] [PubMed]
- Uyama M, Asayama K. Retinal vascular changes in Takayasu disease (pulseless disease), occurrence and evaluation of the lesion. Doc Ophthalmol Proc Ser 1976;9:549-54. [Crossref]
- Noel N, Butel N, Le Hoang P, et al. Small vessel involvement in Takayasu's arteritis. Autoimmun Rev 2013;12:355-62. [Crossref] [PubMed]
- Elizalde J, Capella MJ. Takayasu's retinopathy. Int Ophthalmol 2011;31:533-7. [Crossref] [PubMed]
- Noel N, Butel N, Le Hoang P, et al. Small vessel involvement in Takayasu's arteritis. Autoimmun Rev 2013;12:355-62. [Crossref] [PubMed]
- Nakabayashi K, Nitadori T, Kamiya Y, et al. Atypical Takayasu arteritis: late onset and arthritic manifestations: report of two cases. Int J Cardiol 1998;66 Suppl 1:S221-7; discussion S229.
- Ishikawa K, Maetani S. Long-term outcome for 120 Japanese patients with Takayasu's disease. Clinical and statistical analyses of related prognostic factors. Circulation 1994;90:1855-60. [Crossref] [PubMed]
- Liang P, Tan-Ong M, Hoffman GS. Takayasu's arteritis: vascular interventions and outcomes. J Rheumatol 2004;31:102-6. [PubMed]
Cite this article as: Natraj Setty HS, Reddy B, Srinivas BC, Raghu TR, Kharge J, Patil R, Raj S, Nagesh CM, Manjunath CN. Young lady presented with sudden loss of vision. J Xiangya Med 2019;4:13.