
Is it safe to embolize a central pulmonary artery?—a case report
Introduction
Pulmonary arterial embolization is performed to occlude select pulmonary artery branches in patients with conditions such as pseudoaneurysms, true aneurysms, or arteriovenous malformations (AVMs). Clinically relevant shortness of breath, pulmonary arterial hypertension, recurrent hemoptysis, prevention of life-threatening hemorrhage, prevention of paradoxical embolism (through AVM), are considered indications of treatment (1). In these cases, a segmental or smaller artery is embolized (2-11). Embolization provides the benefit of treating the above-mentioned entities without performing thoracotomy and resection, which require patients be placed under general anesthesia for a surgical procedure. This way, patients who are not candidates for surgery and/or general anesthesia can have potentially fatal condition treated without the morbidity associated with a surgical procedure. To our knowledge, purposeful en bloc pulmonary artery embolization of an entire lung has not been reported.
Case presentation
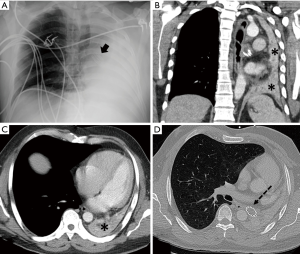
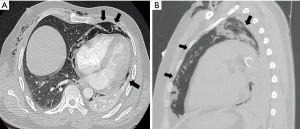
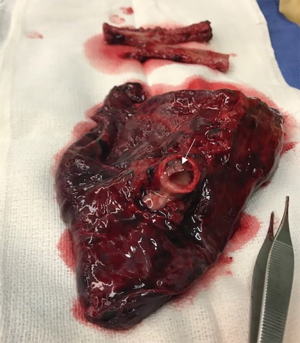
A 42-year-old male with no past medical history presented to an outside facility with chest pain, cough and fever. Work up included a contrast enhanced chest CT, which was significant for complete left lung collapse, presumed secondary to a bronchial mass. Subsequent bronchoscopies and trans-bronchial biopsies were non-diagnostic. Bare metal stent was placed in the left main stem bronchus in attempt to open the collapsed lung. He was subsequently transferred to our institution for further management. Follow-up imaging showed no change in complete collapse of the left lung, ipsilateral mediastinal shift, and new completely occluded left main stem bronchus stent (Figure 1). The collapsed lung tissue demonstrated good contrast enhancement (Figure 1), indicating preserved blood flow. There was no evidence of a pulmonary or mediastinal lesion compressing the bronchus. Repeat bronchoscopy showed completely occluded bronchial stent. Attempts to re-open the stent were unsuccessful. Attempt to remove the stent resulted in bronchial tear and extensive pneumo-mediastinum and subcutaneous emphysema (Figure 2). Cardiothoracic surgery was consulted for further management. The patient had blood oxygen saturation level of 90% on room air. Based on CT images and overall clinical picture, it was determined that the patient’s chest pain and low oxygen saturation was secondary to shunting of blood in the collapsed left lung; and his cough was secondary to an indolent infectious/inflammatory process in the collapsed lung. After a multidisciplinary discussion, a decision was made to perform a left pneumonectomy. He was considered high-risk because of the now distorted anatomy with pulmonary blood flow shunt, presence of bronchial tear, pneumomediastinum and a metal stent in the bronchus. Interventional radiology was consulted for embolization of the left main pulmonary artery. The main aim of en bloc pulmonary artery embolization of the left pulmonary artery was to help reduce bleeding risks during pneumonectomy. A secondary aim was to shut down the shunting of blood in the left lung and to allow pulmonary circulation to adapt to occluded left pulmonary artery prior to pneumonectomy, although this was not critical as pneumonectomy is a well-established surgery that can be safely performed without prior occlusion of pulmonary arteries. Details of the embolization procedure are described in the “Embolization Technique” section below. Following an uneventful embolization of the left pulmonary artery, the patient reported no new symptoms. The patient’s oxygen saturation level slightly improved to 93–94% on room air. Three days after embolization, the patient underwent left pneumonectomy with minimal intra-operative blood loss. The gross specimen is depicted in Figure 3. The postsurgical course was complicated by small left hemothorax, which required thoracotomy and cauterization of a small artery in the chest wall. The remainder of the patient’s hospital course was unremarkable and the patient was subsequently discharged. The exact cause of lung collapse could not be determined even on explant lung pathological examination, which demonstrated no significant interstitial fibrosis, granulomatous inflammation, vasculitis, or mass lesion in lung parenchyma. There was bronchiolitis with foci of organizing fibrosis and granulation tissue. Bronchial cartilage demonstrated no specific pathologic changes. Patient was a construction worker and exposure to toxic fumes or aspiration of toxic fluid was considered the most likely etiology. At 1 year follow-up, his clinical exam was unremarkable, the patient was asymptomatic and his oxygen saturation was 98% on room air compared to 90% prior to embolization and surgery.
Embolization technique
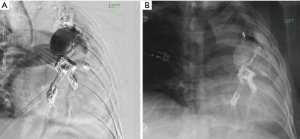
Access was obtained into the left main pulmonary artery via right common femoral vein using angled GLIDECATH (Terumo, Somerset, NJ, USA) and hydrophilic GLIDEWIRE (Terumo, Somerset, NJ, USA). Left pulmonary angiogram was performed using an Omni flush catheter (AngioDynamics, Latham, NY, USA). A 2.8 French Progreat microcatheter (Terumo Somerset, NJ, USA) was coaxially advanced through the GLIDECATH and multiple detachable coils were deployed in the left main pulmonary artery. Few smaller branches arising proximal to the coil mass were selectively embolized, to avoid extending the coil mass into the proximal left main pulmonary artery and therefore avoid difficulty in clamping this artery during surgery. The coils used were standard and soft Ruby embolization coils (Penumbra, Inc., Alameda, CA, USA) and Azur 0.018 inch detachable HydroCoils (Terumo, Somerset, NJ, USA). Figure 4 is the post embolization angiogram showing complete cessation of blood flow in the left pulmonary artery circulation.
Discussion
Pulmonary arterial interventions are used to treat a wide variety of pathologies. Catheter directed or mechanical thrombolysis of pulmonary emboli and angioplasty and/or stenting of stenosed pulmonary arteries are done to restore normal flow through the pulmonary arterial circulation (1). On the other hand, embolization is performed to occlude pulmonary artery branches in patients with conditions such as pseudoaneurysms, true aneurysms, or AVMs. Pseudoaneurysms can be caused by varying pathologies: necrotizing pneumonia, bacterial endocarditis, mucormycosis, tuberculosis, vasculitides (Behcet’s), iatrogenic trauma from Swan-Ganz or Cournard catheters, congenital heart disease, and necrotic cavitary lung carcinoma (1-3,5-10). True pulmonary artery aneurysms are extremely rare and the etiology is still unclear. AVMs are congenital in nature and are treated if they are symptomatic or if the feeding artery is 3 mm or more in diameter. Metallic coils, vascular plugs, acrylic glue, and detachable balloons have been described in the literature as being used to achieve embolization (1-3,9). A percutaneous embolization is typically preferred over surgical resection of such lesions as it is minimally invasive and has very little recovery time.
The case presented in this report is unique in that the pulmonary arterial supply to the entire left lung was closed off by embolization of the left main pulmonary artery. There are previously reported cases of temporary unilateral pulmonary artery occlusion done to perform tests to predict morbidity and mortality prior to pneumonectomy (12,13). However, no cases of irreversible occlusion of a central pulmonary artery were found. In our case, occlusion achieved with embolization coils was irreversible. The embolization helped reduce blood loss during pneumonectomy in this patient who was considered high risk for surgery. Embolization also terminated the effective “shunt” created by a collapsed, non-functioning but well perfused lung. It is important to note that our patient had no other past medical history and his functioning right lung was able to sufficiently compensate for non-functioning left lung. This case demonstrates that it is feasible and safe to permanently embolize the pulmonary arterial supply of an entire lung in carefully selected patients.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2019.05.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pelage JP, El Hajjam M, Lagrange C, et al. Pulmonary artery interventions: an overview. Radiographics 2005;25:1653-67. [Crossref] [PubMed]
- Veeram Reddy SR, Patel VG, Gualano SK. Amplatzer vascular plug IV for occlusion of pulmonary arteriovenous malformations in a patient with cryptogenic stroke. Ann Pediatr Cardiol 2014;7:145-7. [Crossref] [PubMed]
- Markowitz DM, Hughes SH, Shaw C, et al. Transcatheter detachable balloon embolotherapy for catheter-induced pulmonary artery pseudoaneurysm. J Thorac Imaging 1991;6:75-8. [Crossref] [PubMed]
- Cantasdemir M, Kantarci F, Mihmanli I, et al. Emergency endovascular management of pulmonary artery aneurysms in Behçet's disease: report of two cases and a review of the literature. Cardiovasc Intervent Radiol 2002;25:533-7. [Crossref] [PubMed]
- Ferretti GR, Thony F, Link KM, et al. False aneurysm of the pulmonary artery induced by a Swan-Ganz catheter: clinical presentation and radiologic management. AJR Am J Roentgenol 1996;167:941-5. [Crossref] [PubMed]
- Karak P, Dimick R, Hamrick KM, et al. Immediate transcatheter embolization of Swan-Ganz catheter-induced pulmonary artery pseudoaneurysm. Chest 1997;111:1450-2. [Crossref] [PubMed]
- Santelli ED, Katz DS, Goldschmidt AM, et al. Embolization of multiple Rasmussen aneurysms as a treatment of hemoptysis. Radiology 1994;193:396-8. [Crossref] [PubMed]
- Gomez-Jorge J, Mitchell SE. Embolization of a pulmonary artery pseudoaneurysm due to squamous cell carcinoma of the lung. J Vasc Interv Radiol 1999;10:1127-30. [Crossref] [PubMed]
- Renie WA, Rodeheffer RJ, Mitchell S, et al. Balloon embolization of a mycotic pulmonary artery aneurysm. Am Rev Respir Dis 1982;126:1107-10. [PubMed]
- Remy J, Smith M, Lemaitre L, et al. Treatment of massive hemoptysis by occlusion of a Rasmussen aneurysm. AJR Am J Roentgenol 1980;135:605-6. [Crossref] [PubMed]
- Picard C, Parrot A, Boussaud V, et al. Massive hemoptysis due to Rasmussen aneurysm: detection with helicoidal CT angiography and successful steel coil embolization. Intensive Care Med 2003;29:1837-9. [Crossref] [PubMed]
- Laros CD, Swierenga J. Temporary unilateral pulmonary artery occlusion in the preoperative evaluation of patients with bronchial carcinoma. Comparison of pulmonary artery pressure measurements, pulmonary function tests and early postoperative mortality. Med Thorac 1967;24:269-83. [PubMed]
- Ikeda T, Onuki T, Nishiuchi M, et al. Clinical assessment of unilateral pulmonary artery occlusion test with dobutamine infusion. Expansion of surgical indications in patients with primary lung cancer and impaired cardiopulmonary functions. Jpn J Thorac Cardiovasc Surg 2000;48:802-8. [Crossref] [PubMed]
Cite this article as: Hussaini SH, Gupta A, Zhou J, Tak V. Is it safe to embolize a central pulmonary artery?—a case report. J Xiangya Med 2019;4:23.


