
Multiple calcifications in the skin and viscera: a case report
Introduction
Nodular panniculitis, also known as Weber-Christian disease, is a nonsuppurative inflammatory disorder that affects the adipose tissue (1). It presents as symmetrically distributed subcutaneous nodules which are often accompanied by abdominal pain and vomiting as well as systemic symptoms that include fever and malaise. It is classified into dermatologic and systemic types based on the organ systems involved. In this article, we present a rare case of multiple calcifications in the skin and viscera. This is followed by a discussion of the diagnosis and treatment.
Case presentation
A 39-year-old male was admitted to our department with an 8-year history of intermittent abdominal pain localized to the left lower quadrant without radiation. It recurred at intervals ranging from a few days to several months and did not follow a regular pattern with each episode usually lasting for a few minutes. It was colicky in nature without evident alleviating or aggravating factors. It was associated with anorexia, weight loss, and constipation. There was no nausea, vomiting, hematemesis or melena. He noticed subcutaneous nodules in his abdomen and a rash on both lower limbs.
Prior to being admitted to our center, he was evaluated at a different facility after experiencing worsening pain that increased in both frequency and duration over the 4 months prior to presentation. Routine blood tests revealed leukopenia and thrombocytopenia. A diagnosis of “nodular panniculitis” was made for which he received prednisone and leflunomide without significant improvement in his pain. This prompted the patient to discontinue his medications and was then admitted to our center for further diagnosis and treatment.
His past medical history was significant for pulmonary tuberculosis diagnosed at age 17 and was treated. He also experienced recurrent episodes of cellulitis. He had a history of benzene exposure. There was no family history of similar abdominal pain or hematological abnormalities.
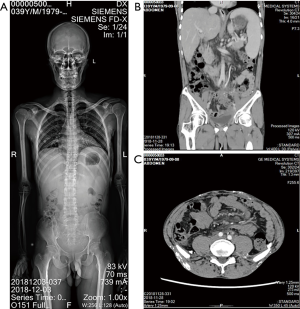
On physical exam, he had multiple subcutaneous nodules with ulcerations affecting the abdomen, perineum and gluteal region (Figure 1). The nodules were firm, mobile, and painless. His abdomen was not tender, and he had no hepatosplenomegaly. The abdominal subcutaneous nodules coalesced, giving the abdomen a board-like consistency.
Part of the laboratory examination results are shown in Table 1. Besides, C-reactive protein (CRP), procalcitonin, and amylase were not elevated. Tests for HIV, syphilis, hepatitis C virus, and hepatitis B virus were negative. Tumor markers were unremarkable. Anti-nuclear antibody (ANA), anti-double-stranded DNA antibody, and autoimmune hepatitis panel were negative. Esophagogastroscopy revealed esophageal varices (grade II) and chronic non-atrophic gastritis. Colonoscopy revealed proctitis with histopathology confirming a chronic mucosal inflammation. Spine X-ray showed multiple calcifications throughout the whole body (Figure 2A). The contrast-enhanced computed tomography (CT) revealed the following: (I) thickened walls of the colon from the hepatic flexure to the rectum with fullness between the lower rectum and the presacral space; (II) splenomegaly; (III) uneven enhancement of hepatic parenchyma in the venous phase; (IV) multiple patchy and strip-like areas with decreased enhancement in splenic parenchyma in the venous phase; (V) possible mesenteric panniculitis with mild haziness of the root of the mesentery; (VI) cholecystitis; (VII) esophageal varices; (VIII) multiple calcifications in the subcutaneous soft tissue of the perianal area; (IX) calcifications in the right lower lung; (X) chronic inflammation in the medial segment of the right middle lung and the lower lingual segment of the left upper lung; and (XI) permanent epiphysis in the anterior edge of the L4 vertebral body (Figure 2B,C).
Table 1
| Item | Result | Reference range |
|---|---|---|
| Blood routine | ||
| WBC | 0.8×109/L | 3.5–9.5×109/L |
| PLT | 40×109/L | 125–350×109/L |
| Granulocyte | 0.0×109/L | 1.8–6.3×109/L |
| Hemoglobin (g/L) | 152.0 | 130–175 |
| Liver function test | ||
| Albumin (g/L) | 33.9 | 40.0–55.0 |
| Total bilirubin (µmol/L) | 27.1 | 1.7–17.1 |
| AST (U/L) | 51.5 | 15.0–40.0 |
| ESR (mm/h) | 55.0 | 0–21 |
| TG (mmol/L) | 1.88 | <1.70 |
WBC, white blood cell; PLT, platelet; AST, aspartate aminotransferase; ESR, erythrocyte sedimentation rate; TG, triglyceride.
Bone marrow biopsy showed hypocellular bone marrow, adipose tissue was relatively proliferative, and hematopoietic tissue significantly reduced.
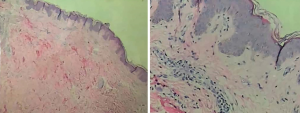
Skin biopsy revealed lymphocyte infiltration around the superficial vessels of abdominal dermis as well as fat necrosis, ghost cells, and calcifications within skin of the right arm (Figure 3).
Genetic analysis revealed a missense mutation in the WAS gene: NM-000377; exon9: p.I294T, c. T881C. This mutation leads to severe congenital neutropenia and thrombocytopenia.
Due to financial difficulties, he did not receive any further treatment and was eventually discharged.
IMDT discussion
Discussion among physicians from Xiangya Hospital Central South University
We conducted intradisciplinary and multidisciplinary consultation of this case. Our patient had multiple subcutaneous nodules (measuring 5–10 mm), and multiple calcifications involving viscera without spontaneous regression and also without symptoms such as fever and sweating. He had no family history of marriage to a close relative. Multiple fibrosis and calcifications were seen in subcutaneous, visceral, and mesenteric adipose tissues. Skin biopsy showed fat necrosis and ghost cells. The possibility of nodular panniculitis was considered. However, whether a rare disease involving multiple systems caused it, should also be considered.
Rheumatologist
Multiple systems were affected in this patient. The amounts of leukocytes and platelets decreased, panniculitis and calcifications were observed in skin, and the anti-Jo-1 antibody was positive in previous laboratory tests. Although the patient had no obvious muscular symptoms, the possibility of dermatomyositis could not be ruled out based on his skin lesions. It is suggested that testing for the antibody profile of dermatomyositis, electromyography, and muscle biopsy should be further performed. Polyarteritis nodosa is an inflammatory disease that involves middle and small arterial war. Different locations of affected arteries lead to various symptoms. It could limit in the skin and manifest subcutaneous nodules distributed along superficial arteries. Elevated antineutrophil cytoplasmic antibodies (ANCA) could be found in serum. Histopathological examination shows necrotic vasculitis affecting all layer of arterial war, without adipose degeneration or necrosis. Gene testing may also be performed if necessary.
Dermatologist
There were diffuse skin calcifications in this patient. While multiple factors including metabolism, immunity, lupus, tumors, and tuberculosis can cause skin calcification, none were identified in this case. Panniculitis was seen in the skin, viscera, and mesentery of this patient, and there was no obvious abnormality in the pancreas. The possibility of α1-antitryptase-associated panniculitis could not be ruled out. Testing for α1-antitryptase is recommended. Whole genome sequencing can also be performed as necessary.
Panniculitis is a broad term that involves inflammation of adipose tissues. Nodular panniculitis is one of the forms of panniculitis, which affects adipose lobule, also called Weber-Christian disease (2). It could present as symmetric multiple subcutaneous nodules, accompanied by the recurrent general malaise, fever and arthralgia, and other systemic symptoms. The different locations of panniculitis associated with symptoms and prognosis of the illness. The most frequent is subcutaneous adipose tissue, followed by liver, spleen, bone marrow, and mesenteric adipose tissue (3). In laboratory examination, it presents as elevating of the inflammatory indexes, such as erythrocyte sedimentation rate (ESR), CRP, and white blood cell counts. Sometimes immune complexes would elevate in serum, may suggest that immunological reaction play a role in nodular panniculitis progression (4). The etiology of nodular panniculitis remains unclear. The typical histopathological features of this disease include degeneration, necrosis and inflammatory cell infiltration of adipose tissues at an early stage, accompanied by vasculitis changes; lately, foam cell was generated by the phagocytosis of macrophages to adipocytes; finally, fibroblast replaces foam cell in the lesion (5). The diagnosis of nodular panniculitis mainly relies on clinical symptoms and biopsy of the lesion and excluded other diseases simultaneously. Corticosteroids and immunosuppressants have proved efficacy in the treatment.
The result of all exon genetic diseases detection and analysis suggest that the patient has WAS missense mutation, which leads to congenital severe neutrophil leukopenia associated with this gene, also known as Wiskott-Aldrich syndrome (WAS). WAS is a rare X-linked primary immunodeficiency characterized by infections, microthrombocytopenia, and eczema. People with WAS are at risk of developing autoimmune disorders and lymphoid malignancies (6,7). The etiology of WAS is due to mutations of the WASP coding gene. WASP is a protein expressed in the hematopoietic system, regulating cytoskeleton (8). WASP signaling triggers cell adhesion and immunological synapsis formation. Thus an abnormal expression of WASP would lead to severe immunodeficiency. It could explain the poor medical condition of our patients, and nodular panniculitis may secondary to his WAS.
Several issues regarding the diagnosis and treatment of this patient were further discussed as follows
Question 1: can the diagnosis of panniculitis be justified?
Expert opinion 1: Dr. Christina Fleming
By definition, panniculitis is a group of diseases the hallmark of which is inflammation of subcutaneous adipose tissue and may present with tender skin nodules and systemic signs, including weight loss and fatigue. In this particular case, the patient developed abdominal pain and had associated abdominal subcutaneous nodules, which were ‘woody’ and tender. There was no association with other known causes of nodular skin conditions (SLE, TB, malignancy) and a previously positive anti-Jo-1 antibody was observed.
Expert opinion 2: Dr. Eli D. Ehrenpreis & Dr. Ahmed Khattab
Panniculitis is a broad term that means inflammation of the adipose tissue. Although the patient’s chief complaint was recurrent abdominal pain, the presence of subcutaneous nodules prompted the authors to consider panniculitis in their differential; and this is justified. The authors did an excellent job exploring the possible etiologies of panniculitides in this patient. They excluded several infectious and inflammatory disorders through history and basic laboratory studies. An essential step in approaching this case that seems to be suffering from a multisystem disease, was histopathology the aim of which is (I) to confirm the presence of inflammation of the subcutaneous fat with minimal involvement of the epidermis, and (II) to classify the inflammation as predominantly septal or predominantly lobular and to further categorized it based on the presence or absence of vasculitis. Although the histopathology did highly suggest the presence of panniculitis, it did not describe whether it was predominantly septal or lobular and did not clearly state the presence or absence of vasculitis. Therefore, it did not provide adequate information to guide narrowing down the differential diagnosis and suggesting treatment. In conclusion, the consideration of panniculitis is justified by the mere presence of scattered subcutaneous nodules; a presumptive diagnosis of panniculitis can be made by the presence of inflammation predominantly in the subcutaneous tissue with minimal involvement of the epidermis; however, histopathology was suboptimal in describing its morphology.
Expert opinion 3: Dr. Lisa Nyberg
The patient had accelerated symptoms in the last 4 months with weight loss, constipation, and abdominal pain. Mesenteric panniculitis is often asymptomatic or associated with mild to moderate symptoms such as local tenderness. Other radiological features seen in mesenteric panniculitis is a pseudocapsule surrounding the mass lesion, hyperattenuation of the adipose tissue and a halo surrounding the nodules, not described here. The generalized disease of this kind is not previously described and not likely in this case. Sclerosing mesenteritis is a more aggressive disease that is associated with weight loss, fever, and high inflammatory markers. The condition described here is severe but do not present with fever or elevated CRP. Nor does it respond to steroid treatment.
Question 2: panniculitis involving viscera is not responsive to hormone therapy. What is your suggestion on treatment?
Expert opinion 1: Dr. Christina Fleming
Anti-inflammatory drugs have been used to treat visceral panniculitis, for example, mesenteric panniculitis, including colchicine, azathioprine, cyclophosphamide, infliximab, and pentoxifylline. The National Organisation for Rare Diseases (NORD) describes the aim of treatment of mesenteric panniculitis as the reduction of mesenteric inflammation and the control of symptoms of the disease. NORD reports successfully the use of thalidomide where a prospective clinical trial has demonstrated that the drug thalidomide improves symptoms and reduces blood levels of ESR and CRP in patients with mesenteric panniculitis. Low dose naltrexone also appears to work by modulating the immune system and increasing circulating levels of enkephalins and endorphins. Hormonal therapies (e.g., tamoxifen) are generally reserved to treat visceral panniculitis where fibrosis is a dominant feature due to their anti-fibrotic abilities.
Expert opinion 2: Dr. Eli D. Ehrenpreis & Dr. Ahmed Khattab
The treatment has to be targeted to the cause of panniculitis. Not enough information was provided to guide further diagnosis and management.
Expert opinion 3: Dr. Lisa Nyberg
Before the cause of the patient’s condition is determined, further immunosuppressants should be avoided, and treatment is given only symptomatically.
Question 3: what diseases cause multiple ectopic calcifications throughout the whole body?
Expert opinion 1: Dr. Christina Fleming
Multiple ectopic calcifications is a rare condition associated with the following disease processes: Sarcoidosis, fibrodysplasia ossificans progressive, non-hereditary myositis ossificans, scleroderma, dermatomyositis and systemic lupus erythematosus.
Expert opinion 2: Dr. Eli D. Ehrenpreis & Dr. Ahmed Khattab
Vascular diseases such as venous insufficiency, Ehlers-Danlos syndrome, and low-flow (cavernous) venous malformations. Calcium-phosphorus related diseases including hypervitaminosis D, milk-alkali syndrome, chronic renal failure with hemodialysis and renal osteodystrophy, and hyperparathyroidism. Autoimmune disorders including dermatomyositis, polymyositis, scleroderma (calcinosis circumscripta), mixed connective tissue disease, and systemic lupus erythematosus. Besides, trauma could lead to multiple ectopic calcifications, like heterotopic ossification and injection granulomas. Infectious diseases, for example, cysticercosis, trichinosis, dracunculiasis, and Armillifer armillatus. Other diseases also could cause such condition, like pseudoxanthoma elasticum, subcutaneous lipodystrophy, calcinosis universalis, sarcoidosis, and idiopathic tumoral calcinosis
Expert opinion 3: Dr. Lisa Nyberg
Extrapulmonary sarcoidosis may affect all organs involved and similarly present itself; s-ACE should be analyzed. The rapid progression, the weight loss, and the low WBC and PLT may raise suspicion towards malignancy and calcifications as a paramalignant phenomenon, sometimes appear before the detectable primary disease. A PET/CT should be considered.
Conclusions
Diagnosis of panniculitis is challenging to justify, needed adequate evidence to exclude other diseases. When patients present as subcutaneous nodules, accompanied by fever or other systemic symptoms, we should not forget the possibilities of nodular panniculitis. Histopathological examination of the lesion is vital for diagnosis and differential diagnosis. Genetic detection may be helpful for diagnosis and further investigation of etiology.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2019.07.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wu F, Zou CC. Childhood Weber-Christian disease: clinical investigation and virus detection. Acta Paediatr 2007;96:1665-9. [Crossref] [PubMed]
- Hagag AA, Barakat AN. Recurrent panniculitis: Weber-Christian disease. Eur J Inflamm 2016;14:113-7. [Crossref]
- Liu H, Chen YD, Wu Y, et al. Nodular Panniculitis with Hemophagocytic Lymphohistiocytosis. Chin Med J (Engl) 2018;131:2860-1. [PubMed]
- Requena L, Sánchez Yus E. Panniculitis. Part II. Mostly lobular panniculitis. J Am Acad Dermatol 2001;45:325-61; quiz 362-4. [Crossref] [PubMed]
- Segura S, Requena L. Anatomy and histology of normal subcutaneous fat, necrosis of adipocytes, and classification of the panniculitides. Dermatol Clin 2008;26:419-24. v. [Crossref] [PubMed]
- Catucci M, Castiello MC, Pala F, et al. Autoimmunity in wiskott-Aldrich syndrome: an unsolved enigma. Front Immunol 2012;3:209. [Crossref] [PubMed]
- Notarangelo LD, Miao CH, Ochs HD. Wiskott-Aldrich syndrome. Curr Opin Hematol 2008;15:30-6. [Crossref] [PubMed]
- Aiuti A, Biasco L, Scaramuzza S, et al. Lentiviral hematopoietic stem cell gene therapy in patients with Wiskott-Aldrich syndrome. Science 2013;341:1233151. [Crossref] [PubMed]
Cite this article as: Li H, Wang M, Lian G, Long X, Fleming C, Ehrenpreis ED, Khattab A, Nyberg L, Peng J. Multiple calcifications in the skin and viscera: a case report. J Xiangya Med 2019;4:31.



