Impact of rest on office blood pressure in patients with hypertension and diabetes at the national obesity centre of Yaounde: a cross-sectional study in Sub-Saharan Africa
Introduction
Hypertension is a major public health problem worldwide, affecting more than a billion people (1,2). Hypertension is defined by the World Health Organization (WHO) as blood pressure (BP) ≥140/90 mmHg at least 2 times on two different occasions (3). This value was recently lowered by the American College of Cardiology (ACC) to a threshold of ≥130/90 mmHg, further increasing the proportion of individuals affected by this disease (4). This figure is expected to increase in the coming years, especially in sub-Saharan Africa (SSA) (5). By 2025, it is estimated that about 1.5 billion of the world’s population will be hypertensive and a hypertension prevalence in United states of America of 46% (3,4). Hypertension is the main cardiovascular risk factor associated with the occurrence of cardiovascular diseases (coronary heart disease, stroke, heart failure). As a result, achieving BP reduction and good hypertension control has a direct effect on the occurrence of cardiovascular (CV) events and CV deaths (6,7).
A few numbers of hypertensive patient achieve a BP control <140/90 mmHg, worldwide and in SSA (8,9). BP reduction (<140/90 mmHg) is the only measurable parameter to affirm hypertension control. BP measurement is the key element for the diagnosis and evaluation of hypertension. It can be performed in the office, as self-measurement, or during ambulatory blood pressure measurement (ABPM). Despite the many recommendations of scientific societies, it is established that BP is not properly measured in practice most of the time (3,10-12). Most of the studies done on hypertension control (in patients with or without diabetes) evaluated the drug or diet efficacy and not the reliability of the BP measurement (9,13,14). It is difficult to differentiate sustained hypertension from white coat hypertension in patients with 5 minutes of rest. Rest (as caffeine consumption and physical exercise) has a recognized influence on BP values (15-17). Recent data suggest that office BP is not reliable for assessing the correct BP (18-20). If a duration of 15 to 30 minutes rest seems to be needed to obtain a reliable BP, just a few works have been carried out to quantify the amount of reduction and the associated factors. This work aims to assess the impact of prolonged rest on the reduction of BP in patients seen in the office and to identify the associated factors.
Methods
Study design and setting
We conducted a cross-sectional study from January to February 2016 in a population of patients with diabetes and hypertension, followed at the National Obesity Centre of the Yaoundé Central Hospital, in Yaoundé, Cameroon, with a population of about 2 million inhabitants. The follow-up of patients at this center is done by endocrinologists and internists.
Participants
We included consenting patients with diabetes and hypertension, of both sexes, aged ≥18 years, seen in the out-patient clinic. Subjects were approached regardless of the duration of diagnosis or follow-up. Pregnant women, non-hypertensive patients, and non-consenting patients were excluded. The sampling was exhaustive. Administrative authorizations were obtained prior to the completion of this study.
Data collection
The screening was conducted by trained medical personnel in the out-patient clinic. All participants were subjected to a face-to-face interview after a signed consent. Data were collected (using a standardized questionnaire) on demographics, smoking habits and alcohol consumption, diabetes and hypertension history including drugs treatment and complications and other cardiovascular risk factors.
The physical examination included BP and anthropometric measurements. BP (systolic and diastolic) were measured in chair-seated patients on the left arm after 15 minutes (BP15), 30 minutes (BP30), and 45 minutes (BP45) of rest. All BP values for a participant were measured by the same medical personnel. BP measurements were performed using automated sphygmomanometers (OMRON, Kyoto, Japan), with appropriate cuff size. Weight (in Kg) was measured in participants on light clothing using an automated scale. Height (in m) was measured using a wooden platform and a height rule. Body mass index was calculated as weight (Kg)/height (m) × height (m). Waist circumference was measured between the iliac crest and the lower rib margin and the hip circumference was measured at the intertrochanteric level. Fasting capillary blood glucose was measured with a One Touch Ultra glucose monitor (Lifescan, Milpitas, California).
Definitions
Hypertension was defined as a BP ≥140 mmHg (systolic) and/or 90 mmHg (diastolic) measured in two separate occasions. Obesity was defined as a BMI of ≥30 kg/m2, and overweight was defined as a BMI between 25 and 29.9 kg/m2. Dyslipidemia was defined as high total cholesterol (≥2.5 g/L), and/or high LDL cholesterol (≥1.3 g/L), and/or low HDL cholesterol (≤0.40 g/L), and/or high triglycerides (≥1.7 g/L). A sedentary lifestyle was defined as the absence of any physical activity (absence of at least 3 walking episodes of 45 min in a week).
Hypertension was considered to be controlled among participants when systolic (and diastolic) BP was <140/90 mmHg. Good diabetic control was defined by HbA1C <7%. Waist circumference >94 cm in men or 80 cm in women was considered to be high (abdominal obesity). Excessive alcohol consumption was based on intake either more than 3 (2 for women) standard glasses of wine per day or more than 10 (5 for women) local beers per week. Traditional alcohol beverage was not assessed. Participants who smoked at least one cigarette per day were classified as current smokers.
Sample size and statistical analysis
A convenient sample of all eligible patients seen during the study period was considered. Data were analyzed using Statistical Package for Social Sciences (SSPS Inc, Chicago, Illinois, USA) V.20.0 software. Results are summarized as counts and percentages for qualitative variables and mean and standard deviation (SD) for quantitative variables. Group comparisons were performed with Chi2 test and student t-test for qualitative variables where applicable, and analysis of variance (ANOVA) for quantitative variables. A P value <0.05 was considered statistically significant.
Results
Characteristics of the study population
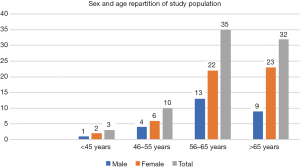
Among the 80 participants enrolled in this study, 53 (67%) were female. The mean age was 62.4 years (range 39–82). The most common age group was 56–65 years (43.8%) (Figure 1). The main cardiovascular risk factors in our study population were hypertension, diabetes, obesity, and dyslipidemia. Smoking was more common among men (P=0.003), while obesity (P=0.002) and overweight were more common among women.
Mean hypertension duration was 6.6±7.6 years. Hypertension duration was more recent among male than female. Ten percent of participants were not any antihypertensive treatment. Renin Angiotensin Aldosterone System (RAAS) blockers (ARB and ACEI) were the most anti-hypertensive drugs used among the participants (65%). The most common combination therapy used was an association of RAAS blockers and calcium channel blocker (CCB). Hypertension treatment and other risk factors are shown in Table 1.
Table 1
| Characteristics | Men | Women | Total | P value |
|---|---|---|---|---|
| n (%) | 27 (33.8) | 53 (66.3) | 80 (100.0) | |
| Mean age (range) | 61.5 (45–73) | 62.9 (39–82) | 62.5 (39–82) | 0.47 |
| Smoking | 5 (18.5) | 0 (0) | 5 (6.2) | 0.003 |
| Duration of hypertension ± SD | 4.8±5.4 | 7.5±8.4 | 6.6±7.6 | 0.14 |
| Duration of diabetes ± SD | 5.8±5.4 | 7.3±6.0 | 6.3±5.6 | 0.27 |
| Number of antihypertensive drugs, n (%) | ||||
| 0 | 4 (14.8) | 4 (7.5) | 8 (10.0) | 0.43 |
| 1 | 6 (22.2) | 18 (34.0) | 24 (30.0) | 0.28 |
| 2 | 13 (48.1) | 20 (37.7) | 33 (41.3) | 0.37 |
| 3 and more | 4 (14.8) | 11 (20.8) | 15 (18.8) | 0.52 |
| Number of antidiabetic drugs, n (%) | ||||
| 0 | 1 (3.7) | 3 (5.7) | 4 (5.0) | 1 |
| 1 | 11 (40.7) | 20 (37.7) | 31 (38.8) | 0.79 |
| 2 | 14 (51.9) | 27 (50.9) | 41 (51.2) | 0.94 |
| 3 | 1 (3.7) | 3 (5.7) | 4 (5.0) | 1 |
| Anti hypertensive treatment, n (%) | ||||
| ACE inhibitors | 13 (48.1) | 29 (54.7) | 42 (52.5) | 0.58 |
| Calcium channel blockers | 13 (48.1) | 26 (49.1) | 39 (48.8) | 0.94 |
| Angiotensine receptor antagonists | 2 (7.4) | 8 (15.1) | 10 (12.5) | 0.81 |
| Diuretics | 13 (48.1) | 23 (43.4) | 36 (45.0) | 0.95 |
| Type of antidiabetic drug, n (%) | ||||
| Insuline | 17 (63.0) | 20 (37.7) | 37 (46.3) | 0.03 |
| Metformine | 19 (70.4) | 40 (75.5) | 59 (73.8) | 0.62 |
| Sulfonylurea | 4 (14.8) | 23 (43.4) | 27 (33.8) | 0.01 |
| Others | 2 (7.4) | 0 (0) | 2 (2.5) | 0.11 |
| Microvascular complications, n (%) | ||||
| All | 17 (63.0) | 32 (60.4) | 49 (61.3) | 0.51 |
| Retinopathy | 7 (25.9) | 14 (26.4) | 21 (26.3) | 0.96 |
| Nephropathy | 6 (22.2) | 2 (3.8) | 8 (10.0) | 0.02 |
| Neuropathy | 17 (63.0) | 31 (58.5) | 48 (60.0) | 0.7 |
| Macrovascular complications, n (%) | ||||
| All | 6 (22.2) | 9 (17.0) | 15 (18.8) | 0.39 |
| Ischemic heart disease | 3 (11.1) | 3 (5.7) | 6 (7.5) | 0.38 |
| Stroke | 0 (0) | 2 (3.8) | 2 (2.5) | 0.55 |
| Peripheral artery disease | 3 (11.1) | 4 (7.5) | 7 (8.8) | 0.68 |
| Dyslipidemia, n (%) | 13 (48.1) | 21 (39.6) | 34 (42.5) | 0.47 |
| Statine use, n (%) | 10 (37) | 27 (50.9) | 37 (46.3) | 0.24 |
| Obesity, n (%) | 9 (33.3) | 37 (68.8) | 46 (57.5) | 0.002 |
| Overweight, n (%) | 11 (40.7) | 20 (37.7) | 31 (38.8) | 0.49 |
| Glycemic control, n (%) | 13 (48.1) | 34 (64.2) | 47 (58.7) | 0.17 |
Mean diabetes duration was 6.3±5.6 years. It was more recent in male than female. More than half of the study population had good glycemic control (58.7%). Metformin (73.8%) was the most used glycemic lowering medication, followed by insulin (46.3%), and sulfonylurea (33.8%). Insulin use is more frequent in male (P=0.032) and sulfonylurea use exhibits a female predominance (P=0.011). Diabetes complications were frequent among study participants. Microvascular complications rate was 61.3%, and macrovascular complications were seen in 18.8% of the study population. Statin use was low (46.8%), compared to the prevalence of dyslipidemia and the global cardiovascular risk of the patients.
Impact of rest on blood pressure measurement and associated factors
The mean SBP30 and SBP45 were significantly low among women than men (P=0.02 and P=0.01 respectively). There was no significant difference in DBP between men and women according to the rest time (Table 2).
Table 2
| Variables | Men | Female | All population | P value |
|---|---|---|---|---|
| SBP15 | 156.0±27.8 | 150.5±23.2 | 152.3±26.4 | 0.38 |
| SBP30 | 151.7±19 | 140.1±21.9 | 144.0±21.6 | 0.02 |
| SBP45 | 146.3±19.5 | 134.7±20.3 | 138.6±20.6 | 0.01 |
| DBP15 | 91.2±17.2 | 87.2±13.6 | 88.5±15.1 | 0.26 |
| DBP30 | 89.3±15.1 | 83.3±12.3 | 85.3±13.5 | 0.06 |
| DBP45 | 84.0±10.5 | 82.3 ±12.2 | 82.9±11.6 | 0.52 |
BP fell after rest by 8.3 (6.5%) mmHg between SBP30 and SBP15 and by 13.5 (9.4%) mmHg between SBP45 and SBP15. By the same, DBP fell by 3.1 (3.9%) mmHg between DBP30 and DBP15 and by 5.5 mmHg (6.6%) between DBP15 and DBP45 (Figure 2). All these reductions were statistically significant (P<0.001).
Only 30% of participants achieved good BP control at 15 minutes. BP45 reclassified 6.3% and 16.3% with poor control at BP30 and BP15 respectively (Figure 3). There was a female predominance among participants controlled at 30 min (P=0.002).
Among all factors tested, RAAS blockers were associated with SBP reduction but only between 30 and 15 minutes (P=0.004) (Table 3). Specifically, ACEI use was associated with SBP reduction (P=0.006 between 30 and 15 minutes, and P=0.04 between 45 and 30 minutes) (Table 4).
Table 3
| Variables | Overall | RAAS+ | RAAS- | P value |
|---|---|---|---|---|
| SBP30-SBP15 | 8.3±15.1 | 4.7±11.9 | 14.7±18.1 | 0.004 |
| SBP45-SBP 15 | 13.5±15.5 | 11.4±12.5 | 17.3±19.5 | 0.10 |
| DBP30-DBP15 | 3.1±6.6 | 2.9±7.2 | 3.6±5.6 | 0.64 |
| DBP45-DBP15 | 5.5±9.7 | 6.2±10.5 | 4.2±7.9 | 0.38 |
BP, blood pressure.
Table 4
| Variables | Overall | ACEI+ | ACEI- | P value |
|---|---|---|---|---|
| SBP30-SBP15 | 8.3±15.1 | 3.9±12 | 13.1±16.8 | 0.006 |
| SBP45-SBP 15 | 13.5±15.5 | 10.2±12.6 | 17.2±17.6 | 0.04 |
| DBP30-DBP15 | 3.1±6.6 | 3.5±7.8 | 2.7±5.2 | 0.56 |
| DBP45-DBP15 | 5.5±9.7 | 6.6±11.4 | 4.4±7.4 | 0.32 |
BP, blood pressure.
Discussion
We carried out this cross-sectional study to assess the magnitude of the reduction of BP with prolonged rest in a group of patients with hypertension and diabetes in a sub-Saharan African setting. We also sought to study the determinants of this reduction. This study represents the first analysis of BP drop with rest in a specific population with hypertension and diabetes in Africa.
This study should be interpreted in the light some limitations. The sample size of participants was small due to the restricted population of diabetics with hypertension, thus reducing our capacity to detect significant correlations. Another problem was our first BP measurement at 15 minutes making difficult the comparison with other studies. Our study population is made up of people with long-standing diabetes (>6 years), and who had many vascular complications. Finally, participants of this study are living, for the majority, with few financial means, making difficult the availability of some drug and the realization of paraclinical examinations.
Mean SBP15 in this study was 152 mmHg. This finding is similar to that reported by Menanga et al. in a population of hypertensive patients in an outpatient clinic in Yaounde after 10 minutes of rest (21). Overall, 24 (30%) participants had their BP controlled at 15 minutes. Our findings are close to that reported by Dzudie et al. after 10 minutes of rest (control rate of 24.6%) (22).
Our findings are similar to those reported in other settings in the world, where there was a BP fall with time (18,19,23,24). We found that rest improved BP reliability on SBP (with a drop of 8.3 mmHg between 15 and 30 minutes and 13.5 mmHg between 15 and 45 minutes) and DBP (with a drop of 3.1 between 15 and 30 minutes a and 5.5 between 15 and 45 minutes). But compared to other studies, the BP fall with time was lower in our participants. At 16 minutes, the BP drop reported by Sala et al. was almost the same by 45 minutes in our study, and at 30 minutes, the BP drop reported by Bos et al. was almost the double that shown in our study at 45 minutes (18,19). This low BP fall could be due to our study population, who were all African diabetic patients with hypertension (living in a Sub-Saharan African setting), and who had many vascular complications. Genetic factors, lifestyle, and environmental factors could also play an important role in BP fall in our population. However, Scherpbier-de Haan et al. findings were similar to our own with a reduction of 7.6 mmHg of SBP and 2.5 mmHg of DBP at 30 minutes (24).
Due to BP fall with rest, BP45 reclassified 6.3% and 16.3% with poor control at BP30 and BP15 respectively. This was similar to that reported by Nikolic et al., where rest improved control by 9.2% (23).
The new finding in this study is the association of SBP reduction partially with the use of Renin Angiotensin Aldosterone System (RAAS) blockers, and specifically with the Angiotensin Converting Enzyme Inhibitors (ACEIs). There is no similar finding in the literature. Further studies are needed to confirm our findings.
Conclusions
With increased resting for 45 minutes, rather than the recommended 5 to 10 minutes, SBP is reduced by 8.3 between 30 and 15 minutes and by 13.5 mmHg between 45 and 15 minutes. DBP is reduced by 3.1 between 30 and 15 minutes and by 5.5 mmHg between 45 and 15 minutes. BP45 reclassified 6.3% and 16.3% with poor control at BP30 and BP15 respectively. ARB and ACE inhibitors seemed linked to a time reduction of SBP. Resting for 45 minutes may improve the reliability of the office blood pressure values in Africans with diabetes and hypertension. Further studies are needed to confirm our findings.
Acknowledgments
This work has been presented at the 10th Congress of the Cameroonian Society of Cardiology, March 2016, Yaoundé, Cameroon.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2019.10.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This work was approved by the institutional board of the Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Cameroon, the Centre Regional Ethics Committee for Human Health research (registration number CE00538/CRERSHC/2016), and the director of the Yaoundé Central Hospital. This work was carried out in accordance with the declaration of Helsinki (as revised in 2013). All ethical rules involving research on disadvantaged groups such as prisoners have been respected. Patients were free to attend the study without any outside constraint. We obtained informed and signed consent form from each participant. There was no participant under 16 years in the study group.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mills KT, Bundy JD, Kelly TN, et al. Global Burden of Hypertension: Analysis of Population-based Studies from 89 Countries. J Hypertens 2015;33:e2. [Crossref]
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021-104. [Crossref] [PubMed]
- Whitworth JAWorld Health Organization, International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 2003;21:1983-92. [Crossref] [PubMed]
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. J Am Coll Cardiol 2018;71:e127-248. [Crossref] [PubMed]
- Twagirumukiza M, De Bacquer D, Kips JG, et al. Current and projected prevalence of arterial hypertension in sub-Saharan Africa by sex, age and habitat: an estimate from population studies J Hypertens 2011;29:1243-52. [Crossref] [PubMed]
- Alderman MH. Blood pressure control to reduce cardiovascular morbidity and mortality: today and tomorrow. Eff Clin Pract 1998;1:23-5. [PubMed]
- Antonakoudis G, Poulimenos L, Kifnidis K, et al. Blood pressure control and cardiovascular risk reduction. Hippokratia 2007;11:114-9. [PubMed]
- Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood PressureThe JNC 7 Report. JAMA 2003;289:2560-72. [Crossref] [PubMed]
- Kingue S, Ngoe CN, Menanga AP, et al. Prevalence and Risk Factors of Hypertension in Urban Areas of Cameroon: A Nationwide Population-Based Cross-Sectional Study. J Clin Hypertens (Greenwich) 2015;17:819-24. [Crossref] [PubMed]
- Frese EM, Fick A, Sadowsky HS. Blood pressure measurement guidelines for physical therapists. Cardiopulm Phys Ther J 2011;22:5-12. [Crossref] [PubMed]
- Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013;31:1281-357. [Crossref] [PubMed]
- Rakotz MK, Townsend RR, Yang J, et al. Medical students and measuring blood pressure: Results from the American Medical Association Blood Pressure Check Challenge. J Clin Hypertens (Greenwich) 2017;19:614-9. [Crossref] [PubMed]
- Patel A. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet 2007;370:829-40. [Crossref] [PubMed]
- SPRINT Research Group. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med 2015;373:2103-16. [Crossref] [PubMed]
- Mahe G, Comets E, Nouni A, et al. A minimal resting time of 25 min is needed before measuring stabilized blood pressure in subjects addressed for vascular investigations. Sci Rep 2017;7:12893. [Crossref] [PubMed]
- Cornelissen VA, Smart NA. Exercise Training for Blood Pressure: A Systematic Review and Meta-analysis. J Am Heart Assoc 2013;2:e004473. [Crossref] [PubMed]
- Turnbull D, Rodricks JV, Mariano GF, et al. Caffeine and cardiovascular health. Regul Toxicol Pharmacol. 2017;89:165-85. [Crossref] [PubMed]
- Sala C, Santin E, Rescaldani M, et al. How Long Shall the Patient Rest Before Clinic Blood Pressure Measurement? Am J Hypertens 2006;19:713-7. [Crossref] [PubMed]
- Bos MJ, Buis S. Thirty-Minute Office Blood Pressure Monitoring in Primary Care. Ann Fam Med 2017;15:120-3. [Crossref] [PubMed]
- Green LA. It is Time to Change How We Measure Blood Pressures in the Office. Ann Fam Med 2017;15:105-6. [Crossref] [PubMed]
- Menanga A, Edie S, Nkoke C, et al. Factors associated with blood pressure control amongst adults with hypertension in Yaounde, Cameroon: a cross-sectional study. Cardiovasc Diagn Ther 2016;6:439-45. [Crossref] [PubMed]
- Dzudie A, Kengne AP, Muna WFT, et al. Prevalence, awareness, treatment and control of hypertension in a self-selected sub-Saharan African urban population: a cross-sectional study. BMJ Open 2012;2:1-10. [Crossref] [PubMed]
- Nikolic SB, Abhayaratna WP, Leano R, et al. Waiting a few extra minutes before measuring blood pressure has potentially important clinical and research ramifications. J Hum Hypertens 2014;28:56-61. [Crossref] [PubMed]
- Scherpbier-de Haan N, van der Wel M, Schoenmakers G, et al. Thirty-minute compared to standardised office blood pressure measurement in general practice. Br J Gen Pract 2011;61:e590-7. [Crossref] [PubMed]
Cite this article as: Simeni Njonnou SR, Tiodoung Timnou A, Etoa Etoga MC, Musa Jingi A, Boombhi J, Nganou-Ngnindjo CN, Hamadou B, Mfeukeu-Kuate L, Ndongo Amougou S, Ntsama Essomba MJ, Kengni Kebiwo O, Dehayem Yefou M, Ashuntantang G, Sobngwi E. Impact of rest on office blood pressure in patients with hypertension and diabetes at the national obesity centre of Yaounde: a cross-sectional study in Sub-Saharan Africa. J Xiangya Med 2020;5:2.