
Myocardial bridging mimicking Wellens’ syndrome
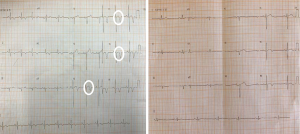
A 60-year-old man presented to the emergency department complaining of recent onset angina at moderate efforts. The resting electrocardiogram (ECG) showed biphasic plus-minus T waves in the precordial leads, compatible with type A Wellens’ syndrome (Figure 1). The cardiac troponins sets were all negatives and resting cardiac echocardiogram was unremarkable. A recent coronary angiography revealed a mid-left anterior descending (LAD) myocardial bridging (MB) with massive systolic compression (Figure 2), without any significant lesions. After optimization of medical treatment (beta-blocker and calcium channel antagonist) the ECG pattern surprisingly changed (Figure 1).
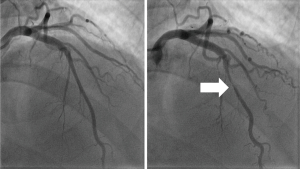
A MB is described as a segment of an epicardial coronary artery that develops a transient intramyocardial course. Generally without repercussion, it may cause angina, arrhythmias, myocardial ischemia and even sudden cardiac death. The burden of ischemia correlates directly with the degree of systolic compression. As in the present case, most MB is found in the mid LAD (1). First-line management for MB is optimal medical treatment with beta-blockers and calcium channel blockers, causing diastolic prolongation. Nitrates cause reflex tachycardia and are therefore contraindicated. In exceptional refractory cases, surgical or percutaneous strategies can be pursued (1,2).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2020.01.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ambesh P, Sharma D, Kapoor A, et al. Unusual Sign from an Unusual Cause: Wellens' Syndrome due to Myocardial Bridging. Case Rep Cardiol 2018;2018:3105653. [Crossref] [PubMed]
- Kaplanis I, Michas G, Arapi S, et al. Myocardial bridge as a cause of pseudo-Wellens' syndrome. Hellenic J Cardiol 2017;58:453-5. [Crossref] [PubMed]
Cite this article as: Pederçole GL, Oliveira MDP, Moritz MA, Cury RBB, Caixeta A. Myocardial bridging mimicking Wellens’ syndrome. J Xiangya Med 2020;5:6.


