
Midventricular type of Takotsubo (stress) cardiomyopathy concurrent to severe coronary vasospasm
Takotsubo (stress) cardiomyopathy (TSC) is defined by transient left ventricular (LV) dysfunction with a variety of wall-motion abnormalities (1,2). Generally recognized as a benign disorder, it predominantly affects elderly women and is often preceded by emotional and/or physical triggers, but has also been reported without evident ones (3,4). Clinical presentation, electrocardiographic findings and cardiac biomarker profiles are often similar to those of acute coronary syndromes (3).
Among 1,750 patients of The International Takotsubo Registry (www.takotsubo-registry.com), the most common variant was the apical (81.7%), followed by midventricular (14.6%), basal (2.2%) and focal (1.5%) types (3,4).
Catecholaminergic imbalance appears to play a pivotal role for TSC occurrence, and reports of concurrency with coronary artery vasospasm have suggested possible common pathways (5-8).
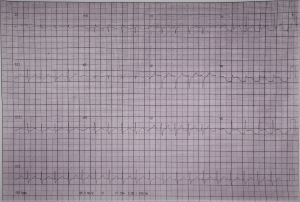
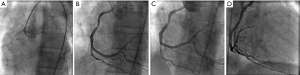
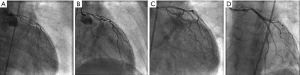
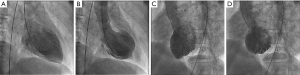
A 49-year-old woman, current smoker, with anxiety disorder and major depression under psychiatric treatment, just after general anesthetic induction to surgical vascular repair of chronic mesenteric ischemia, developed an episode of ventricular fibrillation, promptly reverted with electrical therapy and cardiopulmonary resuscitation. Pre-operative adenosine myocardial perfusion scintigraphy was unremarkable. The 12-lead electrocardiogram just after return of spontaneous circulation showed ST-segment elevation in leads V4–V6 (Figure 1). In addition, she degenerated to severe hemodynamic collapse, stabilized with increasingly doses of norepinephrine and dobutamine. Emergency coronary angiography showed unexpected severe and diffuse right coronary artery (RCA) vasospasm (Figure 2A), precluding complete filling of the artery, mimicking its occlusion. Following selective intracoronary injection of nitroglycerin (400 µg), the normal dominant RCA was then revealed (Figure 2B,C,D). Left coronary system showed a similar pattern of diffuse (but not so severe) vasospasm (Figure 3A,B), also ameliorated after intracoronary nitrate (Figure 3C,D), without any significant stenosis. Left ventriculography on right anterior oblique view (Figure 4A,B) and left anterior oblique view (Figure 4C,D) showed akinesia of all mid portions of anterior, inferior, lateral and septal LV walls, compatible with midventricular type of TSC. Transthoracic echocardiogram (TTE) confirmed those findings. Just after the procedures, still on the cath lab table, there were two new episodes of cardiac arrest (ventricular fibrillation and torsades de pointes ventricular tachycardia), once again promptly reverted. At the intensive cardiac care unit, about 24 hours later, she was already without invasive mechanical ventilatory support, inotropes nor vasopressors, with normal neurological status and no recurrence of arrhythmias. New TTE 4 days later confirmed the initial findings. Cardiac magnetic resonance performed one week after the onset revealed preserved LV ejection fraction, despite hypokinesia of mid segments of all LV walls, without evidence of myocardial infarction. The patient was discharged home at ninth day, with optimal medical treatment (aspirin, rosuvastatin, ramipril and diltiazem), without recurrence of adverse cardiac events. TTE performed four weeks later revealed complete reversal of initial midventricular systolic dysfunction.
The exact pathophysiological mechanism of TSC is still unknown. Neuro-cardiac action with coronary artery vasospasm, like in the present case, may play a special role (8). The spectrum of TSC is wide and ranges from low to very high risk in the acute phase. The relatively rapid recovery of LV function and a selection bias of previous reports toward low-risk patients generated the misapprehension that it is a universally benign disease. This condition, however, represents an acute heart failure syndrome with substantial morbidity and mortality (3).
Acknowledgments
Funding: None.
Footnote
Peer Review File: Available at http://dx.doi.org/10.21037/jxym-20-90
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym-20-90). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hurst RT, Prasad A, Askew JW 3rd, et al. Takotsubo cardiomyopathy: a unique cardiomyopathy with variable ventricular morphology. JACC Cardiovasc Imaging 2010;3:641-9. [Crossref] [PubMed]
- Medeiros K, O'Connor MJ, Baicu CF, et al. Systolic and diastolic mechanics in stress cardiomyopathy. Circulation 2014;129:1659-67. [Crossref] [PubMed]
- Templin C, Ghadri JR, Diekmann J, et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med 2015;373:929-38. [Crossref] [PubMed]
- Oliveira MD, Navarro EC, Ferraz RP, et al. Focal type of the Takotsubo (stress) Cardiomyopathy. J Cardiol & Cardiovasc Ther 2019;12:555850.
- Pelliccia F, Kaski JC, Crea F, et al. Pathophysiology of Takotsubo Syndrome. Circulation 2017;135:2426-41. [Crossref] [PubMed]
- Pelliccia F, Sinagra G, Elliott P, et al. Takotsubo is not a cardiomyopathy. Int J Cardiol. 2018;254:250-3. [Crossref] [PubMed]
- Vilela E, Silva M, Guerreiro C, et al. Takotsubo syndrome and coronary vasospasm: Two faces of the same coin? Indian Heart J 2018;70:455-8. [Crossref] [PubMed]
- Brennan A, Adams H, Galligan J, et al. Coronary vasospasm and concurrent Takotsubo cardiomyopathy. Br J Cardiol 2019;26:38-40.
Cite this article as: Oliveira MDP, Caixeta A. Midventricular type of Takotsubo (stress) cardiomyopathy concurrent to severe coronary vasospasm. J Xiangya Med 2020;5:31.


