
Diagnosis and management of free-floating filling defect in carotid artery—a case report
Introduction
Free-floating filling defect (FFFD) in carotid artery is a relative rare condition. The reported incidence varies from 0.05% to 0.7% based on different studies (1,2). The pathological nature of the filling defect may be ulcerated plaque, intimal flap or free-floating thrombus (3,4). Ischemic cerebrovascular events may occur in over 90% of patients with free-floating thrombus (5). So FFFD can cause disastrous consequences, but the optimal treatment strategy remains controversial. We present the following article/case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jxym-20-91).
Case presentation
From May 2015 to January 2017, we identified 5 patients with FFFD in carotid artery in cardiovascular surgery department of China-Japan Friendship Hospital and People’s Hospital of Xing’an League. All these patients were identified with carotid ultrasound and treated with carotid endarterectomy (CEA) or carotid artery stenting (CAS).
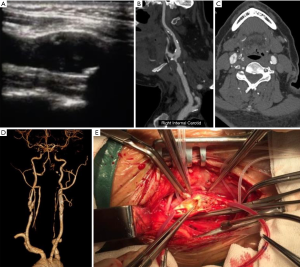
Case 1: a 59 years old male patient admitted on November 2016 with dizziness and right tinnitus for 2 years. Ultrasonography showed >90% carotid artery stenosis with FFFD in carotid artery for 1 day. The patient has a history of coronary artery disease for 10 years. He has received coronary artery bypass grafting in 2008 and percutaneous coronary intervention in 2015. He also has hypertension for 13 years and takes metoprolol to control blood pressure. CEA was carried out for the patient, ulceration of the plaque could be seen during the surgery (Figure 1). After surgery the patient recovered uneventfully.
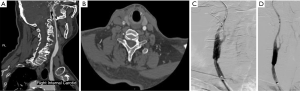
Case 2: a 71 years old male patient with dizziness for 3 years. He has a history of hypertension and diabetes mellitus for more than 10 years. Four years ago, the patient received right CEA and patch angioplasty. Computed tomography (CTA) showed ipsilateral carotid artery FFFD at the proximal part of patch. For this patient we carried out CAS and the result was good (Figure 2).
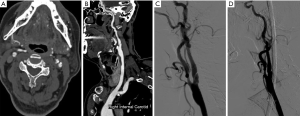
Case 3: a 69 years old male patient with dizziness and tinnitus for 2 years. The patient received radical gastrectomy for gastric cancer 4 years ago. He has no history of hypertension, diabetes mellitus or cardiovascular disease. CTA showed FFFD in carotid artery. We performed CAS for this patient. The dizziness and tinnitus relieved after CAS (Figure 3).
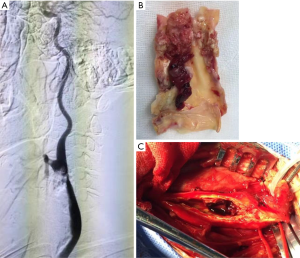
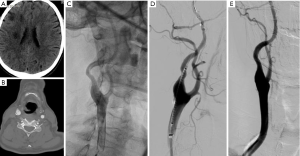
Case 4: a 56 years old male admitted because of transient amaurosis fugax for 1 month. Ultrasonography found >90% carotid artery stenosis with FFFD in carotid artery for 4 days. The patient has a history of hypertension for 20 years and hyperlipidemia for 16 years. Four years ago, the patient has suffered from right stroke and recovered without sequelae. Digital subtraction angiography (DSA) showed FFFD in the distal part of common carotid artery. We carried out CEA for this patient, ruptured plaque and thrombosis can be seen during the surgery (Figure 4). No perioperative complication occurred for this patient.
Case 5: a 60 years old male. The patient was asymptomatic, FFFD in right carotid artery was found in routine physical examination with carotid ultrasonography. the patient has a history of hypertension for 2 years and right stroke for 1 year. He also has a history of intracranial cerebrovascular intervention. CTA showed FFFD in carotid artery and we carried out CAS for this patient (Figure 5). No perioperative complication was observed.
Discussion
FFFD was relative rare and most associated literatures were case reports, among which the largest series consisted of 29 patients (6). However, with the improvement of understanding and development of ultrasonography, the detection of FFFD gradually increased. Funaki et al. identified 21 mobile plaques among 228 patients with carotid artery stenosis with ultrasonography (7). Among the 5 patients in our institution, all were detected by carotid ultrasonography. 4 cases received DSA and 2 failed to display the FFFD. The typical ultrasonographical performance was described by Kume et al. as Jellyfish sign with filling defect in the carotid artery rising and falling in a manner inconsistent with pulsatile carotid artery wall motion (8,9).
The etiology and natural history of FFFD remains unknown. Most are relevant to intimal flap, plaque rupture and subsequent thrombosis (10-13). In 2 cases treated with CEA, we can find 1 was ruptured plaque and 1 was ruptured plaque with thrombus formation. And some FFFD may have relationship with prior surgery or interventional operation. In our study series, 1 patient have received CEA previously and the filling defect was found in the proximal part of the patch. For these patients, the filling defect may be intimal flap and we chose CAS to immobilize the flap. Another patient has received interventional operation for intracranial cerebrovascular disease. The FFFD in this patient may be associated with iatrogenic injury (14). Complete endarterectomy and fixation of the distal intima during CEA and careful management during interventional operation may be important for the prevention of FFFD formation.
It was reported that ischemic cerebrovascular events occurred in most of the cases with FFFD, the pathological basis may be the fall off and embolization of floating substance (15). In our 5 patients, 4 suffered from symptoms including stroke, TIA and other ischemic symptoms. The optimal treatment strategy for FFFD remains controversial. Some investigators recommended anticoagulation and/or antiplatelet treatment for asymptomatic patients (16,17). Delgado et al. (18) reviewed 20 patients, among which 11 received CEA, 2 received CAS and 7 received medical treatment. Funaki et al. (7) identified 21 patients with carotid mobile plaque, all of them were treated with CEA. We prefer to deal with these patients more aggressively to prevent ischemic cerebrovascular events. The exact method depends on the pathological component. When thrombus was suspected, CEA is more suitable. During the procedure, common carotid artery should be clamped first to prevent thrombus fall off. If preoperative examination excluded thrombus, CAS can be a feasible alternative with its minimally invasive nature (19,20).
In conclusion, free-floating filling defect in carotid artery is a typical phenomenon for unstable carotid plaque. Subsequent thrombus formation and collapse can cause ischemic cerebrovascular events. Both CEA and CAS can achieve good curative effect in certain cases, but the optimal treatment strategy need further investigation.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jxym-20-91
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym-20-91). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Arning C, Herrmann HD. Floating thrombus in the internal carotid artery disclosed by B-mode ultrasonography. J Neurol 1988;235:425-7. [Crossref] [PubMed]
- Biller J, Adams HP Jr, Boarini D, et al. Intraluminal clot of the carotid artery. A clinical-angiographic correlation of nine patients and literature review. Surg Neurol 1986;25:467-77. [Crossref] [PubMed]
- Tanriverdi U, Kizilkilic O, Ince B. Huge Free-Floating Thrombus in the Internal Carotid Artery. J Stroke Cerebrovasc Dis 2017;26:3029-30. [Crossref] [PubMed]
- Lane TR, Shalhoub J, Perera R, et al. Diagnosis and surgical management of free-floating thrombus within the carotid artery. Vasc Endovascular Surg 2010;44:586-93. [Crossref] [PubMed]
- Bhatti AF, Leon LR Jr, Labropoulos N, et al. Free-floating thrombus of the carotid artery: literature review and case reports. J Vasc Surg 2007;45:199-205. [Crossref] [PubMed]
- Buchan A, Gates P, Pelz D, Barnett HJ. Intraluminal thrombus in the cerebral circulation. Implications for surgical management. Stroke 1988;19:681-7. [Crossref] [PubMed]
- Funaki T, Lihara K, Miyamoto S, et al. Histologic characterization of mobile and nonmobile carotid plaques detected with ultrasound imaging. J Vasc Surg 2011;53:977-83. [Crossref] [PubMed]
- Kume S, Hama S, Yamane K, et al. Vulnerable carotid arterial plaque causing repeated ischemic stroke can be detected with B-mode ultrasonography as a mobile component: Jellyfish sign. Neurosurg Rev 2010;33:419-30. [Crossref] [PubMed]
- Schlachetzki F, Hoelscher T, Lange M, et al. Ultrasound finding of a mobile atheroma in the common carotid artery. Circulation 2000;102:E105 [Crossref] [PubMed]
- Toelen C, Goverde P, Van Hee R. Dissection of the common carotid artery: a case report. Acta Chir Belg 2009;109:224-7. [Crossref] [PubMed]
- Ferrero E, Ferri M, Viazzo A, et al. Free-floating thrombus in the internal carotid artery: diagnosis and treatment of 16 cases in a single center. Ann Vasc Surg 2011;25:805-12. [Crossref] [PubMed]
- Johnson SP, Fujitani RM, Leyendecker JR, et al. Stent deformation and intimal hyperplasia complicating treatment of a post-carotid endarterectomy intimal flap with a Palmaz stent. J Vasc Surg 1997;25:764-8. [Crossref] [PubMed]
- Ferrero E, Ferri M, Gaggiano A, et al. Free floating thrombus developed on a residual carotid intimal flap after carotid endarterectomy. Diagnosis and treatment. Ann Vasc Surg 2010;24:573-4. [Crossref] [PubMed]
- Mussa FF, Towfigh S, Rowe VL, et al. Current trends in the management of iatrogenic cervical carotid artery injuries. Vasc Endovascular Surg 2006;40:354-61. [Crossref] [PubMed]
- Jaberi A, Lum C, Stefanski P, et al. Computed tomography angiography intraluminal filling defect is predictive of internal carotid artery free-floating thrombus. Neuroradiology 2014;56:15-23. [Crossref] [PubMed]
- Szendro G, Sabetai MM, Tegos TJ, et al. Mobile carotid plaques: the natural history of two asymptomatic and non-operated cases. J Vasc Surg 1999;30:357-62. [Crossref] [PubMed]
- Combe J, Poinsard P, Besancenot J, et al. Free-floating thrombus of the extracranial internal carotid artery. Ann Vasc Surg 1990;4:558-62. [Crossref] [PubMed]
- Delgado MG, Vega P, Roger R, Bogousslavsky J. Floating thrombus as a marker of unstable atheromatous carotid plaque. Ann Vasc Surg 2011;25:1142.e11-7. [Crossref] [PubMed]
- Chakhtoura EY, Goldstein JE, Hobson RW. Management of mobile floating carotid plaque using carotid artery stenting. J Endovasc Ther 2003;10:653-6. [Crossref] [PubMed]
- Parodi JC, Rubin BG, Azizzadeh A, Bartoli M, Sicard GA. Endovascular treatment of an internal carotid artery thrombus using reversal of flow: a case report. J Vasc Surg 2005;41:146-50. [Crossref] [PubMed]
Cite this article as: Zhang J, Zhou Z, Fan X. Diagnosis and management of free-floating filling defect in carotid artery—a case report. J Xiangya Med 2021;6:8.


