A simple behavior change communication package for school children improves lifestyle of rural Bangladeshi students
Introduction
Global data on mortality and morbidity of children and adolescents indicate that children and adolescents have significant needs for health promotion, prevention and health care services (1). According to the World Health Organization (WHO) Global Health Estimates, over 1.7 million children and adolescents aged 5–19 years died in 2016. Most of these deaths occurred due to causes that could either have been treated or prevented. In addition to the lifestyle related diseases, many diseases or conditions could be linked with unsafe water, sanitation, inadequate hygiene (2). Children and adolescents are exposed to these risks leading to severe health consequences during adulthood (3).
Promoting healthy behaviors during adolescence and taking steps to better protect young people from health risks are critical for the prevention of health problems in adulthood, and for countries’ future health and ability to develop and thrive (4). Schools are better place to start with promoting healthy behavior. Globally, over 80% of children in the lower secondary school age are enrolled in school (5). Schools are places where the lifestyle of the students are shaped. In addition, effective school health programme contributes to improve the health of students, school personnel, families of students and other members of the community at large (6,7). Therefore, its effective implementation can bring about a change towards improving the socio-economic condition of a nation (8,9).
It has been reported from Bangladesh that a brief intervention of school children with oral health education can significantly improve knowledge, attitude and practice on oral health (10,11). The commonly used school-based interventions are targeted for communicable diseases control. However, there are evidences that interventions for control of non-communicable disease (NCD) risk factors in schools are also effective (8,12,13). There are evidences that nudging can improve usefulness of the school-based behavior change communications (BCC) (14).
School health programme in Bangladesh has been mandated for school health promotion. Although Health Promoting Schools (HPS) initiative has been undertaken in 1980s based on the principles of Ottawa Declaration in 1986 (15), hardly there has been any HPS initiative in Bangladesh. There are only 23 school health clinics (16) under the school health programme in a country having hundreds of thousands of schools and millions of students. Therefore, the programme is compelled to be inadequate to face the demand of the millions of school children. As a result, the school health programme is providing clinical services only.
We, therefore designed to provide a BCC package that included: (I) building and campus cleanliness, (II) supply of water and soap, (III) BCC materials for students, (IV) training of teachers, and (V) engagement of the local communities. The initiative aimed examining whether the BCC package is useful to improve environment in schools and healthy behavior among the school students.
Methods
Settings
Bangladesh had seven administrative divisions till end of 2015. We have done this study in seven purposively selected secondary schools of seven divisions of Bangladesh. The Bureau of Health Education (BHE) is the central body under the Directorate General of Health Services to create public awareness in general (17). The BHE identified seven local non-governmental organizations (NGOs), and organized several planning meetings with the NGOs and WHO in May 2014. In addition to relevant officials from school health programme, NCD Control programme collaborated to the initiative. NGO directors along with two counselors from their respective organizations participated for uniform understanding of their roles and responsibilities. Then third party had done the baseline and endline assessment among all students who were presented on that day of assessment. There were 2,148 and 2,454 students at baseline and endline assessments, respectively. Almost all teachers (n=91) of seven schools participated in executing the BCC and took part in the evaluation.
The assessment tools
The assessment tools were developed in Bangla and quality of the tool was checked by the relevant experts. Database of teachers and students of the school were prepared using record sheets. Another record/observation sheet was used to record about the playgrounds’ cleanliness and presence of cigarette butts, availability of water supply/tube well in the school campus, toilets, etc. The third one was a questionnaire on health and hygiene aspects including the frequencies of brushing teeth last 30 days, hand-washing frequencies before meal and after defecation for last 30 days, intake of added salt while taking meal, and number of days fruit and vegetables, soft drinks and energy drinks in last seven days, number of days participated in sports, smoking and smokeless tobacco intake. The information on diarrheal disease in last 30 days was also included. The final questionnaire was for collecting opinion of the teachers about the usefulness of the intervention given using self-rated Likert scale options.
The intervention package
We used here a combined approach of creating a supportive psycho-physical environment in the school campuses beyond what is taught in the class room. Additionally, we considered nudging effect of soap and water supply as has been done by others (14). The package included: (I) building and campus cleanliness including supply of water and soap, (II) BCC package for students, and (III) teachers training including community engagement.
Fourteen full time employees of the NGOs (two from each) were trained by the BHE with support from WHO for two days at the beginning and another day to refresh their knowledge and skills. The NGOs in collaboration with the district officials of the BHE organized meetings with management committees of the schools. The importance of (I) cleanliness of the building and campus including playground, supply of water and soap to the toilets, hanging health related posters, informing parents were discussed in the meetings; (II) teachers were oriented for one day about the components of this intervention so that they can teach the students, and (III) teachers took the messages to the students in their routine classes. Assistance was sought from the NGOs for community engagement, as and when needed.
Assessments at base-line and end-line
Both baseline and end-line assessments were done using same questionnaire/ assessments tools. The observation checklist and students survey were done by a third party after receiving necessary training from BHE and WHO (August 2014). Completed survey records were reviewed for their completeness and correctness on the same day. Finally, these were transferred to the BHE. Another round of surveys using the observation checklist, students survey and teachers’ opinion pool were done (September 2015).
Data analysis
The data were analyzed using Epi-info version. 7.1.5.2. The Chi-square test was performed to compare percentages of variables at baseline and end-line.
Ethical consideration
BHE is the central body of the Government of Bangladesh for health promotion for all citizens of the Country. In line with BHE’s mandate the ethics and programme committee has given approval before concluding agreement with the NGOs. To inform the schools management committees and the community at large, concerned NGO organized meetings and orientations with teachers and the community leaders including union council members. They organized free medical camps to provide treatment to the people of the area.
Written informed consent was obtained from both school management committees and teachers of the schools. Consents of the union councils were ensured before launching the intervention. Finally, verbal informed consent was obtained from all participants (students) in line with the principles recommended by the Bangladesh Medical Research Council.
Results
Boys and girls from all seven schools participated in the assessment (Baseline: boys 1,047, girls 1,101; Endline; boys 1,140, girls 1,314). The mean age of the students was 13.4 years in both endline and baseline survey. There was substantial improvement of hygienic conditions in most of the schools. Five to seven (depending on the indicators) schools had clean class rooms, premises, playgrounds, supply of soap and water in the toilets, hanging of health-related posters, supply of drinking water compared to one to three schools at baseline. On the other hand, spit marks of areca nut chewing with betel quid, visible smoking and unhealthy food vendors almost disappeared from the schools.
Schools organized exercise and sports at the end-line more frequently than baseline (exercise 98.4% vs. 73.5%, sports 91.0% vs. 81.3%) (Table 1). Teachers taught importance of hand washing 98.3% vs. 67.7%), dietary salt reduction (85.5% vs. 52.6%), harmful effect of tobacco (96.1% vs. 64.6%) and water-borne disease (98.1% vs. 66.5%) more than before.
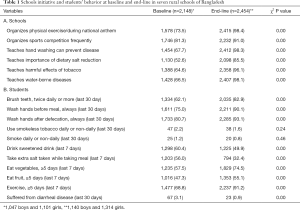
Full table
In general, the lifestyle factors among students at the beginning were far from being satisfactory. For example, only 62.1% students brushed teeth twice a day, 75.0% washed hands always before taking a meal, 80.7% used water and soap for hand washing after using toilet (Table 1). Frequency per week of lifestyle factors (brushing teeth, hand washing before meal and after toilet, dietary salt, exercise, fruit and vegetable intake, sweetened carbonated drinks and participation in sports) improved significantly (P=0.00) but smoking and smokeless tobacco use did not improve. The occurrence of diarrheal has declined significantly (P=0.00) from 3.1% to 0.9%.
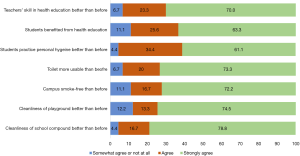
After the end-line survey an opinion poll was conducted among the teachers. Almost 87.8% to 95.6% teachers did agree or strongly agree that the intervention was useful in terms of cleanliness of premises including playground, usable toilets, and there has been a substantial improvement in the students’ behavior. Additionally, 93% teachers felt that they have earned more skills on health education than before (Figure 1).
Discussion
The HPS initiative places significant emphasis on empowering students and building their capacities in health behaviors, and knowledge. This is where students can have a key role in running their schools’ physical and mental environment; and linking with community groups, to collectively address health impacting issues (18). Empowering students and the management committees, is not a task just to measure their understanding or knowledge rather a matter of practice. Any initiative like this one brings an extra burden to the teachers who must make it a part of their routine charter of actions. Although there are challenges, engaging the communities through school management committees and children themselves could be very useful. Therefore, the teachers must have a shift of focus from exclusive class room approach to whole of society approach. Management committees should play an empowering role to facilitate teachers and students’ healthy behavior.
The HPS concept has been developed out of a few international charters like WHO’s Global School Health Initiative (6), Ottawa Charter for Health Promotion (15) and the Jakarta Declaration of the Fourth International Conference on Health Promotion (19). Ideally an HPS should address all the components including policy and strategy development. We could address only a few of them: (I) behaviors affecting health, (II) quality of the physical and psychosocial environment, and (III) school health program implementation. However, these are the areas that can be influenced by BCCs for students in short term. Policies and strategies should be in place for long-term and sustainable benefits.
Our baseline survey findings on brushing teeth, always washing hand before meal and after defecation is similar to the Global School-based Student Health Survey Bangladesh, 2014 (20). However, findings on smoking was very different probably because all our schools are from rural areas where parental guidance is still visible. It is necessary to establish relationships between home and school involving students, teachers and parents/guardians to create a better psychosocial environment. In addition, our results are comparable to Haque et al. (10) and Furukawa et al. (11) that simple intervention can improve oral hygiene practices, and Dreibelbis et al. (14) that nudging behavior change could be a good supplement to BCC. Similar experience has been reported form Austria (21)-and elsewhere. Therefore, our intervention can be claimed as an evidence for the relevant authority to undertake such measures in secondary schools.
The challenges include involvement of two sectors (education and health) for jointly undertaking and evaluating school health initiative. Even within the health sector there are issues of coordination to be developed among child and adolescent health, communicable and NCDs, nutrition, school health programmes and the BHE. There is some reasonable evidence, now, to undertake HPS initiative in a bigger scale in Bangladesh.
In conclusion, a package of BCC intervention could provide substantial positive changes, within a year, in the behavior of the students. The intervention could result in decreased occurrence of diarrheal diseases. Teachers also could develop their relevant skills for HPS. They found the intervention very useful. However, the usefulness of the package in longer term needs to be determined.
Acknowledgments
The survey was conducted by the support of following organizations and people: (I) NGO directors (Barendra Unnayan Sangstha, Community Health and Development Programme, Eklashpur Center for Health, Eco Social Development Organization, Nalta Hospital Community Health Foundation, Reliant Women Development organization, Mukti Associates); (II) school management committees, teachers and students (Chiknagul High School, Islampur High School, Nalta High School, Belgharia Abdus Sattar School, Ekhlaspur High School, Rampasha Islamia High School and Ashrafganj Dhimukhi High School); (III) NCD programme of Health Directorate (for providing educational materials and training of counselors); (IV) WHO (Dr. Mahfuzur Rahman Bhuiyan, Mr. Mohammad Moniruzzaman, Dr. Syed Mahfuzul Huq) and BHE (Health Education Officers of respective districts where the schools are located). They are gratefully acknowledged for their support.
Funding: This intervention was implemented with technical and financial assistance of the World Health Organization Country Office for Bangladesh (WHO reference: 2014/407549-0 and 2015/530916-0).
Footnote
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jxym-20-100
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym-20-100). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The authors alone are responsible for views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization. Global Standards for Health Promoting Schools-Concept Note. [cited 2020 May 12] Available online: http://origin.who.int/maternal_child_adolescent/adolescence/global-standards-for-health-promoting-schools.pdf
- World Health Organization. Don’t pollute my future! The impact of the environment on children’s health; 2017 [cited 2020 May 12]; Available online: http://www.who.int/ceh/publications/don-t-pollute-my-future/en/
- Mills JE, Cumming O. The impact of water, sanitation and hygiene on key health and social outcomes: Review of Evidence; 2016 [ cited on 19 Sept 2020]. Available online: https://www.unicef.org/wash/files/The_Impact_of_WASH_on_Key_Social_and_Health_Outcomes_Review_of_Evidence.pdf
- World Health Organization. Adolescents: health risks and solutions; 2018. [cited 2020 May 12] Available online: https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions
- UNICEF. Statistics Education: secondary education. [cited 2020 May 8]; Available online: https://data.unicef.org/topic/education/secondary-education/
- World Health Organization. Regional Office for the Western Pacific; 1996. Regional guidelines: development of health-promoting schools - a framework for action. Manila: WHO Regional Office for the Western Pacific. [cited 2020 May 12]; Available online: https://apps.who.int/iris/handle/10665/206847
- Nutbeam D, Clarkson J, Phillips K, et al. The health-promoting school: organisation and policy development in welsh secondary schools. Health Educ J 1987; [Crossref]
- World Health Organization. Health Promoting School: an effective approach for early action on NCD risk factors; 2017 [cited 2020 May 11]; Available online: http://www.who.int/healthpromotion/publications/health-promotion-school/en/
- Domitrovich CE, Bradshaw CP, Greenberg MT, et al. Integrated models of school-based prevention: Logic and theory. Psychol Sch 2010;47:71-88. [Crossref] [PubMed]
- Haque SE, Rahman M, Itsuko K, et al. Effect of a school-based oral health education in preventing untreated dental caries and increasing knowledge, attitude, and practices among adolescents in Bangladesh. BMC Oral Health 2016;16:44. [Crossref] [PubMed]
- Furukawa Y, Yokota F, Maruf RI, et al. School-based educational intervention to improve children’s oral health-related behaviors in rural Bangladesh. South East Asia Journal of Public Health 2017;7:27-33. [Crossref]
- Ray M, Guha S, Ray M, et al. Cardiovascular health awareness and the effect of an educational intervention on school-aged children in a rural district of India. Indian Heart J 2016;68:43-7. [Crossref] [PubMed]
- Mondal R, Sarker RC, Acharya NP, et al. Effectiveness of health education-based conventional intervention method to reduce noncommunicable diseases risk factors among rural population. Cardiovasc Diagn Ther 2019;9:30-4. [Crossref] [PubMed]
- Dreibelbis R, Kroeger A, Hossain K, et al. Behavior change without behavior change communication: nudging handwashing among primary school students in Bangladesh. Int J Environ Res Public Health 2016;13:129. [Crossref] [PubMed]
- World Health Organization. 1986. The Ottawa Charter for Health Promotion. WHO Regional Office, Ottawa. [cited 2020 April 28]; Available online: https://www.who.int/healthpromotion/conferences/previous/ottawa/en/
- Directorate General of Health Services. Health Bulletin 2013 [Internet]. Dhaka; 2014 [cited 2020 May 12]; Available online: https://dghs.gov.bd/images/docs/Other_Publication/HB 2013 final - Full version 1March14.pdf
- Bureau of Health Education. School health program [ cited 2020 Sep 5]. Available online: http://bhe.dghs.gov.bd/?p=39
- Barnekow RV, Buijs G, Clift S, et al. Health-promoting schools: a resource for developing indicators. Copenhagen: WHO Regional Office for Europe; 2006. [cited 2020 May 8]; Available online: https://apps.who.int/iris/handle/10665/107805
- World Health Organization. Jakarta Declaration on Leading Health Promotion into the 21st Century; 1997. [cited 2020 May 8]. Available online: https://www.who.int/healthpromotion/conferences/previous/jakarta/declaration/en/
- Report of first Global School-based Student Health Survey (GSHS), Bangladesh, 2014. New Delhi: World Health Organization; 2018. World Health Organization, Regional Office for South-East Asia and National Centre for Control of Rheumatic Fever and Heart Diseases, Ministry of Health and Family Welfare, Dhaka, Bangladesh: [cited 2020 April 28]. Available online: https://nada.searo.who.int/index.php/catalog/33
- Adamowitsch M, Gugglberger L, Dür W. Implementation practices in school health promotion: findings from an Austrian multiple-case study. Health Promotion Int 2017;32:218-30. [Crossref] [PubMed]
Cite this article as: Zaman MM, Rahman MM, Akanda MAW, Hassan AFMK, Khan MRH, Akter S, Akter MK. A simple behavior change communication package for school children improves lifestyle of rural Bangladeshi students. J Xiangya Med 2021;6:4.