
Ischemic colitis involving the right-side colon: clinical case report and diagnostic considerations
Introduction
Ischemic colitis is the most common form of gastrointestinal ischemia. It is due to mesenteric vascular occlusion, stenosis or systemic relative blood volume insufficiency, resulting in insufficient or blocked blood flow to the colon, which in turn induces intestinal ischemia, gangrene and subsequent infection. The disease usually occurs in people over the age of 50 and may be cured with medicine or surgery. Most patients have a good prognosis. However, when the lesion extends to the right colon, the disease progresses rapidly. It is required to make a rapid prognosis of the disease. Clinicians rely more on clinical manifestations and colonoscopy in the diagnosis of ischemic colitis. However, most patients with infection, gangrene, peritonitis, or a serious underlying disease can’t tolerate invasive procedures such as colonoscopy. It makes early pathological diagnosis difficult to implement. In recent years, studies have found that some diseases and physiological states may be related to ischemic colitis. These high-risk factors can assist clinicians in early diagnosis and treatment. Herein, we report a case of ischemic colitis involving the right-side colon, record the transformation of diagnostic ideas as the patient’s condition changes. This case study also demonstrates the importance of risk factor analysis in the early diagnosis of ischemic colitis. We present the following case in accordance with the CARE reporting checklist (available at https://jxym.amegroups.com/article/view/10.21037/jxym-21-37/rc).
Case presentation
A 61-year-old man was admitted to our emergency department with right upper quadrant pain for 11 hours, nausea, vomiting and fatigue. The patient admitted to having a 30-year history of smoking but denied other diseases, except for the diagnosis of eczema 5 years ago. He had been prescribed numerous unknown drugs rather than regular treatment, with no improvement in the rash. Physical examination showed stable vital signs, mild tenderness in the right upper quadrant but no rebound tenderness. Bowel sounds was within normal limits. The rectal examination had been performed with no special findings. There were scattered red rashes on his limbs, some of which have been crusted.
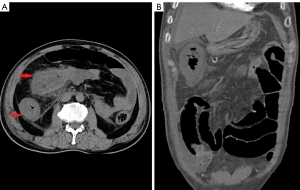
His laboratory examination suggested inflammatory reaction with leukocytosis of 13.49×109/L [reference range, (3.5–9.5) ×109/L], Neutrophil ratio of 82.80% (reference range, 40–75%), which accompanied by a significant increase in D-dimer with 4 times higher than the normal. Abdominal computed tomography (CT) scan revealed diffuse submucosal edema ranging from terminal ileum to the middle of the transverse colon with peritonitis, marked thickening of the walls in descending colon and sigmoid colon (Figure 1).

We suspected the diagnosis of ischemic colitis, based on a combination of clinical manifestations, radiographic and laboratory studies. The patient was empirically initiated on anticoagulant therapy and advised to undergo colonoscopy. However, worsening abdominal pain forced the cancellation of colonoscopy. Computed tomography angiography (CTA) of mesenteric artery was subsequently undergone that revealed no initial evidence of superior or inferior mesenteric artery thrombosis. The diffuse edema in the terminal ileum, ascending colon and transverse colon had no significant change compared with the previous examination, but the thickening of descending colon and sigmoid colon wall was slightly improved, attributed to anal canal decompression (Figure 2A,2B). However, it was too early to rule out ischemic disease. More information from other aspects were needed to support our conjecture. Ischemic colitis risk assessment on the patient had been done. In subsequent screening, we found that this patient was in a high-risk group of ischemic colitis with smoking and recurring rashes. Although he denied a history of other diseases, diabetes screening confirmed that he was a diabetes with glycosylated hemoglobin above normal. Despite the lack of conclusive evidence, we inferred that this patient was most likely to be an intestinal ischemic disease, and the condition might deteriorate in a short period of time.
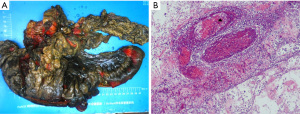
Three days after the supportive care, the patient’s abdominal pain turned to be intolerable, bowel sounds disappeared, the diarrhea continued and generalized tenderness, rebound tenderness and guarding were evolved. Laboratory studies disclosed a significant increase in inflammatory markers compared to his previous presentation on admission. A diagnostic celiac puncture had been performed immediately and extracted of 10 milliliters of bloody ascites. We decided to perform an urgent exploratory laparoscopy on this patient, with a 10-cm mass found in the proximal hepatic curvature of the transverse colon. Eventually the patient had a radical right hemicolectomy and transverse colon left hemicolectomy with temporary colostomy. Pathological findings showed that the serosa of colon and ileum were dark red with the local intestinal adhesion macroscopically. Microscopic examination revealed a massive venous thrombosis in the submucosa of the resected colon with mucosal necrosis, submucous hemorrhage or edema (Figure 3A,3B).
Three days after the operation, the patient began a fluid diet. He was discharged two weeks later. Unfortunately, the patient did not return to the hospital for follow-up, and we were unable to follow him up.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Abdominal pain and Hematochezia are clinical manifestations of almost all diseases involving the colon and rectum, such as inflammatory bowel disease (IBD), tuberculosis (TB), and colorectal tumors. These diseases usually develop slowly. IBD is more common in adolescents. Most people with intestinal TB have a history of infection with TB bacteria in other organs. In addition to abdominal pain, some people may have night sweats and fever. The patient was a 61-year-old man who had abdominal pain for only 11 hours and was progressing rapidly. We don’t think he was coinciding with any of the above diseases. Preliminary examination revealed inflammation of his right colon and an abnormally elevated D-dimer. All signs point to the need to be on the lookout for thromboembolic diseases. Gastrointestinal ischemia is more common in the elderly and may present as chronic refractory abdominal pain or acute abdominal pain with peritoneal irritation. Ischemic colitis is the most common form of gastrointestinal ischemia, accounting for 75% of gastrointestinal ischemic cases (1). The incidence of ischemic colitis is about 15.6/100,000 person-year (2,3). This data may be underestimated for its wide spectrum of clinical symptoms, non-specificity of clinical and laboratory tests. A relative or absolute lack of blood supply to the colon leads to mucosal necrosis and ulceration of the colon, which in turn causes abdominal pain and mucous blood stools. The progression and severity of ischemic colitis disease depends on the site, rate, and extent of ischemia in the colon.
Most colonic ischemia occurs in the left-side, they usually have a good prognosis. But when lesion involves the right-side colon, patients may have a higher surgery rate and in-hospital mortality. This is related to the frequently lack of a well-developed network of marginal collateral vascular and abnormal marginal vascular development in the right colon (1). ACG Clinical Guideline considers CT the main technique for the non-invasive diagnosis of ischemic colitis (4). It can suggest location and illustrate the complications (5), but is not diagnostic of or able to predict complications (2). Colonoscopy may be the best method. It is regarded as the gold standard for confirmation of ischemic colitis. Allowing perform biopsies and histological analysis of the lesion is its greatest advantage. Colonic blood flow is affected by systemic circulation or the anatomy or function of local mesenteric vasculature. The conditions leading to colon ischemia can be classified mainly into two categories: occlusive or a non-occlusive cause (6). Colonoscopy is the first choice for the diagnosis of ischemic colitis, regardless of the causes. It is recommended to be performed within 48 hours of symptom onset for the greatest diagnostic yield (2). Colonoscopy is generally safe. Some existing studies have not explicitly identified ischemic colitis as a risk factor of perforation in colonoscopy (2). However, it is accepted that colonoscopy should be avoided to decrease risk of perforation and avoid deterioration of ischemic colitis, when signs of peritonitis are present. As the patient in the case developed obvious peritonitis on the course of the disease, colonoscopy was not a wise choice at the moment.
Ischemic colitis is thought to be mainly caused by a non-occlusive acute change in colonic microvasculature. Angiography or CTA is barely helpful, since large vessel occlusion is unlikely to be found in most cases (6). Whereas, when there is involvement of the right-side colon, a small number of patients could be identified a vascular event. CTA are the main techniques for the non-invasive diagnosis of mesenteric ischemia, especially for acute mesenteric ischemia (AMI) with a sensitivity of 93% and a specificity of 96% (7). We expected there would be positive findings by CTA, but the results were disappointing. However, it was too early to rule out ischemic disease, for CTA is not effective in displaying small vascular branches. Ischemic colitis often occurs in older people, who may have different underlying diseases. Ischemic colitis complications or the patient’s underlying disease may prevent early colonoscopy from being performed. As mentioned above, imaging examinations do not always reveal the full extent of the disease. We need more evidence to help with the diagnosis.
Patients with ischemic colitis usually have identifiable risk factors. A recent study of 80 patients showed that patients with older than aged 60 years, diabetes, hypertension, hypoalbuminemia, smoking, hypercoagulable states, vascular disease, deep vein thrombosis and constipation are at higher risk of developing ischemic colitis (7). Besides, the usage of some drugs also has been associated with ischemic colitis (5). When colonoscopy is difficult to perform, risk factor analysis can be helpful in clinical diagnosis. It also helps clinicians implement empiric therapy and early detection of complications.
In this case, the patient was a tobacco addicts and had plagued by a recurrent rash in the past 5 years. It is common accepted that tobacco abuse may be responsible for occurrence of ischemic colitis (2). In this case, we inferred that the rash may also be a risk factor. Khazizov and Nodova had conducted a study about the effects of severe rashes on hemostatic systems in patients, which confirms the existence of hypercoagulation processes during the period of active clinical symptoms in patients with severe chronic dermatoses (eczema, atopic dermatitis, psoriasis) (8). The patient mentioned that the rash had become more severe a month before the onset of abdominal pain. Severe forms of rashes might aggravate the abnormal blood coagulation, leading to a hypercoagulable state. Diabetes is also a potential risk factor. Those bad habits and potential diseases might cause vascular damage while making a state of increased coagulability, which aggravated the risk of thrombus and induced microcirculatory disturbance. Some studies have suggested diabetes mellitus and involvement of the right-side colon may to be predisposing factors for a poor prognosis (1,9,10). Ischemia of the colon can result from innumerable causes. To be sure, venous occlusion was the main causes in the case, since pathologists found multiple venous thrombosis in the resected tissue. But it could not be considered that non-occlusive causes, including septic shock, heart failure, cardiac arrhythmias, hemodialysis and medications, had nothing to do. Over the past 6 months, the patients had tried a variety of treatments for the aggravated rash, including using many unknown herbs and informally produced drugs. The lack of pharmacological data made it difficult for us to judge whether drugs abuse was associated with the disease. Occlusive causes and non-occlusive causes might have contributed to the occurrence of the disease at the same time.
Early diagnosis of ischemic colitis has always been a difficult problem, most of the challenges come from its unspecific clinical manifestations. It is difficult to associate common symptoms such as abdominal pain and hematochezia with intestinal ischemia. When the patient’s condition deteriorates sharply, leaving us with limited thinking time, it is more likely to lead to misdiagnosis. In the case, although ischemic colitis had been considered, there was still a lack of direct evidence for an accurate diagnosis. It was not an exception, indeed, only a few of cases can obtain meaningful diagnostic information by colonoscopy at an early stage. Most ischemic colitis is found pathologically after autopsy or surgery. When it seemed to be in a dilemma, we should analyze the high-risk factors of ischemic colitis in patients. Although this could not be used as direct evidence, it does help us to assess the progress of the disease and to intervene timely.
Conclusions
Ischemic colitis is not a rare disease for clinicians, but early diagnosis and intervention are challenging. When the lesion involving the right-side colon, only a small number of patients can get an accurate diagnosis with sharp deterioration of condition. For patients with unexplained abdominal pain and hematochezia, the high-risk factors of thrombus and intestinal ischemia should be evaluated routinely. Ischemic colitis is usually a self-limited disease but about 14% to 66% of patients need surgery (11). For highly suspicious patients, the diagnosis of ischemic colitis can’t be easily ruled out, even if colonoscopy or other tests do not perform successfully, or if the test does not provide a diagnostic opinion. These patients should undergo an ischemic colitis risk factor analysis. If the patient has multiple risk factors, they can be managed for clinical symptoms according to the ischemic colitis principles of care. On the basis of conservative treatment, we should closely observe the changes of the disease, identify the danger signals as soon as possible, and intervene in time.
Acknowledgments
Thanks to Dr. Xiu-Rong Wu for imaging analysis and interpretation.
Funding: This work was supported by the Medical and Health Guiding Project of Xiamen (3502Z20214ZD1028).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jxym.amegroups.com/article/view/10.21037/jxym-21-37/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jxym.amegroups.com/article/view/10.21037/jxym-21-37/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Medina C, Vilaseca J, Videla S, et al. Outcome of patients with ischemic colitis: review of fifty-three cases. Dis Colon Rectum 2004;47:180-4. [Crossref] [PubMed]
- Nikolic AL, Keck JO. Ischaemic colitis: uncertainty in diagnosis, pathophysiology and management. ANZ J Surg 2018;88:278-83. [Crossref] [PubMed]
- Tadros M, Majumder S, Birk JW. A review of ischemic colitis: is our clinical recognition and management adequate? Expert Rev Gastroenterol Hepatol 2013;7:605-13. [Crossref] [PubMed]
- Di Grezia G, Gatta G, Rella R, et al. MDCT in acute ischaemic left colitis: a pictorial essay. Radiol Med 2019;124:103-8. [Crossref] [PubMed]
- Theodoropoulou A, Koutroubakis IE. Ischemic colitis: clinical practice in diagnosis and treatment. World J Gastroenterol 2008;14:7302-8. [Crossref] [PubMed]
- Doulberis M, Panagopoulos P, Scherz S, et al. Update on ischemic colitis: from etiopathology to treatment including patients of intensive care unit. Scand J Gastroenterol 2016;51:893-902. [Crossref] [PubMed]
- Menke J. Diagnostic accuracy of multidetector CT in acute mesenteric ischemia: systematic review and meta-analysis. Radiology 2010;256:93-101. [Crossref] [PubMed]
- Khazizov IE, Nodova ES. A pathogenetic study of the hemostatic system in patients with severe forms of eczema, atopic dermatitis and psoriasis (a review of the literature and the authors’ own data). Ter Arkh 1993;65:43-9. [PubMed]
- Barouk J, Gournay J, Bernard P, et al. Ischemic colitic in the elderly: predictive factors of gangrenous outcome. Gastroenterol Clin Biol 1999;23:470-4. [PubMed]
- Longo WE, Ballantyne GH, Gusberg RJ. Ischemic colitis: patterns and prognosis. Dis Colon Rectum 1992;35:726-30. [Crossref] [PubMed]
- Tseng J, Loper B, Jain M, et al. Predictive factors of mortality after colectomy in ischemic colitis: an ACS-NSQIP database study. Trauma Surg Acute Care Open 2017;2:e000126. [Crossref] [PubMed]
Cite this article as: Huang DL, Wang X, Huang WF. Ischemic colitis involving the right-side colon: clinical case report and diagnostic considerations. J Xiangya Med 2022;7:9.


