Early total care for open lateral ankle dislocation without tearing of tibiofibular sindesmosis: case report
Highlight box
Key findings
• Open ankle dislocation; distal fibula fracture; tibio-fibular syndesmosis; early total care; case report.
What is known and what is new?
• Ankle joint dislocation is a relatively frequent injury at a young age and occurs following high-energy trauma or sports trauma.
• Pure open dislocation of the ankle or dislocation not accompanied by rupture of the tibiofibular syndesmosis ligaments is an extremely rare injury.
What is the implication, and what should change now?
• A detailed assessment, including the patient history, imaging examinations and classifications is necessary for a timely diagnosis and treatment. The choice of the early total care demonstrated to be a good option with mechanical ankle stability and good mobility.
Introduction
Ankle joint dislocation is a relatively frequent injury at a young age and occurs following high-energy trauma or sports trauma (1). The treatment depends on the extent of the trauma, and consists on an immediate reduction, preferably in sedation, and a subsequent immobilization of the joint using a brace or an external fixator in case of concomitant fractures (2). Pure open dislocation of the ankle or dislocation not accompanied by rupture of the tibiofibular syndesmosis ligaments is an extremely rare injury. We report a clinical case deals with an open lateral dislocation of the ankle joint without tearing of the tibiofibular syndesmosis ligaments accompanied by a complex fracture of the mid-foot, following a motorcycle accident. This trauma was urgently treated through joint reduction and stabilization with an external fixator, a cannulated screw at fibula level and K-wires for the stabilization of the fracture of the fifth and fourth metatarsal bones. We present the following case in accordance with the CARE reporting checklist (available at https://jxym.amegroups.com/article/view/10.21037/jxym-22-16/rc).
Case presentation
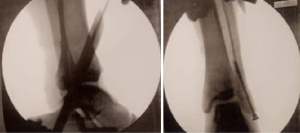
A 16 years-old patient, which presented at the orthopedic emergency room of the Santa Misericordia Hospital in Perugia, Italy, following a motorcycle accident, in which he encountered a high-energy trauma in the left lower limb. The physical examination revealed about ten centimeters of exposed dislocation of the ankle joint, classified as a Gustilo-Anderson 2A (Figure 1), pain with functional limitation, and no neurological and major vascular deficits, confirmed by a triphasic ultrasonographic Doppler. The radiographic examination reported an exposed dislocation of the tibio-talar joint, with fibula fracture, classified as a Weber B one, a displaced distal diaphyseal fracture with dislocation of the base of the fifth metatarsal bone, and fracture of the base of the fourth metatarsal bone (Figure 2). A computed tomography (CT) examination with three dimensions (3D) reconstruction was performed (Figure 3). Due to the open nature, an antibiotic prophylaxis with piperacillin/tazobactam 3 g, amikacin 1 g, metronidazole 400 mg, was performed, in order to let the patient undergoing to emergency surgical treatment. A loco-regional anesthesia was adopted; ten liters of physiological solution was used for the washing of the wound, and a subsequent manual reduction of the dislocation under amplioscopic control was performed; thus, the fibula was definitively synthetized by a 60 mm cannulated screw and the joint was stabilized with a Hoffman II external bridge fixator (External Fixation System, Stryker), a device which consisted in two fiches on 4 mm to the level of the tibial shaft and a trans-calcaneal fiche. Subsequently, under amplioscopic control, reduction of the dislocation of the V metatarsus was achieved by two 1.8 mm K wires, which was fixed on the cuboid bone, and a definitive percutaneous synthesis with intramedullary K wire of the fracture of the fifth metatarsal bone was gained. At the last intraoperative amplioscopic control, a stable synthesis was satisfactorily obtained (Figure 4).

The patient remained in the trauma department for one week, in order to control the clinical condition and the soft tissues state continuing the antibiotic therapy with piperacillin/tazobactam 500 mg and ampicillin/sulbactam 3 g.
At the discharge, non-weight-bearing and the use of two crutch for 30 days, weekly dressings of the fixator device and wounds, left lower limb in anti-declive position with strengthening of quadriceps muscles, deep vein thrombosis prophylaxis and pain relief therapy with opioid drugs were recommended. The wound dressings were performed with physiological solution at the level of the K-wires and the fiches of the external fixator, and wound margins underwent cruentation with a subsequent application of Iruxol® ointment and Ligasano® polyurethane-soft-foam dressing medication.
One month after surgery, the patient underwent to radiographic follow-up: early development of bone callus was noted (Figure 5); moreover, pain symptoms relief, absence of vascular and neurological deficits, and wound healing by secondary intention were reported. At this follow-up, the patient was allowed to walk with partial weight-bearing using two crutches. Two months after the trauma, another clinical-radiographic control was performed: further development of callus compared to the previous control was noted (Figure 6) and it was decided to remove the fixation devices. At the time of this follow-up neither local pain nor tenderness, and no functional limitations were reported. After removal of the synthesis devices, the ankle appeared stable after stress tests. Thus, the patient was allowed to walk with progressive weight bearing using two crutches, and to wear a walker brace for 20 days. Three months after the trauma, the patient walked autonomously without the use of a brace, with no analgesic functional limitations; the clinical follow-up showed a loss of 10 degrees in ankle extension and pain and tenderness at the acupressure of the fifth metatarsal bone, American Orthopaedic Foot and Ankle Society (AOFAS)’s equal to 75 (3). Radiographic examination showed complete bone healing of the fibula, but a malunion at the level of the distal shaft of the left fifth metatarsal bone. Consequently, one cycle of magnetic fields (BIOSTIM, Igea, Carpi, Italy) at those bone level, specific physiotherapy for the complete recovery of the joint range of motion, and new clinical and radiographic follow-up after another month were recommended. At the three-month follow-up, a reduced tone of the periarticular muscles of the ankle was noted, probably due to prolonged immobilization of the joint. Radiographs showed poor healing of the left fifth metatarsal fracture, with an unresolved malunion of the bone stumps (Figure 7). However, despite these radiological findings, the patient detected good clinical conditions, and the mind-foot pain symptoms resolved and at the ankle joint was stable in the stress and stability tests. Therefore, the patient was suggested to progressively resume sporting activity, to perform strengthening of the ankle muscles and to undergo a further clinical and radiographic control three months thereafter. At the last follow-up, the patient reported fully resumed daily living and sports activities, on physical examination the joint appeared stable in the stress tests which excluded any unrecognized lesions of the deltoid ligament, reaching an AOFAS score of 95, despite at the radiographic control non-union at the diaphysis of the fifth metatarsus was reported (Figure 8).

Ethical statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parent for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Open dislocation of the ankle not accompanied by rupture of the tibiofibular syndesmosis ligaments is an extremely rare injury. To our knowledge, there have been few reports in the English-language literature (4). Furthermore, open ankle dislocation with fracture are less common than closed ones, that are the most common intra-articular injuries of weight-bearing joints: they represent a challenge for surgeon, either in acute or in the late outcomes (5). In the current clinical case, since an open dislocation associated with a distal fibula fractures occurred, it had been important to fully assess the integrity of the soft tissues and the vascular and nervous conditions (6). Once dealing with the clinical evaluation of the patients, it was possible to rely on various classification systems, ranging from the type of mechanism (i.e., Lauge-Hansen classification), the integrity of the soft tissues both in closed traumas (i.e., Oestern and Tscherne classification) and in those exposed (i.e., Gustilo and Anderson classification), or the fracture pattern and the possible involvement of the syndesmosis (i.e., AO and Denis-Weber classifications) (6-9). It has been so important to quickly choose the type of treatment that must restore capsule-ligament stability, ensure healing of fractures, and prevent complications, either in acute, referable to early vascular-nerve injuries, such as the development of infections or late infections associated with osteonecrosis, residual capsule-ligamentous instability, mal- or non-unions, heterotopic ossifications of the joint capsule, and osteoarthrosis (10). Delayed repositioning is a negative prognostic factor: the urgent recommendation for repositioning prior to admission remains; this is to avoid consequential injuries and a deterioration of the functional result. However, risks must be carefully assessed (11).
Since this was an uncommon injury, there was no standard treatment protocol in the literature, which showed that many different treatments have been applied for open ankle fractures in the last decades (4,5).
This case report presented a peculiarity which could appear to run against to the principles of emergency treatment. In fact, the choice was to use an external fixator, associated with a cannulated screw to stabilize the distal fibula fracture, in consideration of the state of the soft tissues and the risks of a definitive synthesis with plaque, which would have increased both the infection probability rate at the bone level and the healing of the tissues themselves. Furthermore, the compromised skin did not allow us to predict the timing of a second stabilization, as another risk which could compromise definitive outcomes. Therefore, the association of a damage control treatment, with early total care approach, ensured an ideal compromise between the quality of syntheses and the reduction of complications (12,13).
Our surgical choice gave excellent clinical results and patient reported satisfaction, despite the non-healing of the fracture of the distal shaft of the V metatarsus.
As reported in the literature, other authors supported this kind of treatment; Al-Obaidi et al. evaluated the results of fibular synthesis in closed and open ankle fractures, and concluded that minimal synthesis could give good results both in open and closed fractures (14). This surgical option was also shared in the work of Xiao et al., in which authors stated that external fixation combined with minimal invasive fixation (i.e., screws or K-wires) in open ankle fractures was less traumatic, thus facilitating bone healing (15).
Open lateral ankle dislocation without tearing of the tibio-fibular syndesmosis ligaments is an extremely rare injury. A detailed assessment, including the patient history, imaging examinations and classifications is necessary for a timely diagnosis and treatment. The choice of the early total care demonstrated to be a good option with mechanical ankle stability and good mobility.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jxym.amegroups.com/article/view/10.21037/jxym-22-16/rc
Peer Review File: Available at https://jxym.amegroups.com/article/view/10.21037/jxym-22-16/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jxym.amegroups.com/article/view/10.21037/jxym-22-16/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parent for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kawai R, Kawashima I, Tsukada M, et al. Treatment of open ankle dislocation without associated fractures in a young athlete using external fixation and ligament repair with suture tape augmentation. BMC Musculoskelet Disord 2020;21:351. [Crossref] [PubMed]
- Wight L, Owen D, Goldbloom D, et al. Pure Ankle Dislocation: A systematic review of the literature and estimation of incidence. Injury 2017;48:2027-34. [Crossref] [PubMed]
- Kitaoka HB, Alexander IJ, Adelaar RS, et al. Clinical Rating Systems for the Ankle-Hindfoot, Midfoot, Hallux, and Lesser Toes. Foot Ankle Int 1997;18:187-8. [Crossref] [PubMed]
- Demiralp B, Komurcu M, Ozturk C, et al. Acute traumatic open posterolateral dislocation of the ankle without tearing of the tibiofibular syndesmosis ligaments: a case report. J Am Podiatr Med Assoc 2008;98:469-72. [Crossref] [PubMed]
- Ye T, Chen A, Yuan W, et al. Management of grade III open dislocated ankle fractures: combined internal fixation with bioabsorbable screws/rods and external fixation. J Am Podiatr Med Assoc 2011;101:307-15. [Crossref] [PubMed]
- Lawson KA, Ayala AE, Morin ML, et al. Ankle Fracture-Dislocations: A Review. Foot & Ankle Orthopaedics 2018;3:2473011418765122. [Crossref]
- Tartaglione JP, Rosenbaum AJ, Abousayed M, et al. Classifications in Brief: Lauge-Hansen Classification of Ankle Fractures. Clin Orthop Relat Res 2015;473:3323-8. [Crossref] [PubMed]
- Yim GH, Hardwicke JT. The Evolution and Interpretation of the Gustilo and Anderson Classification. J Bone Joint Surg Am 2018;100:e152. [Crossref] [PubMed]
- Oliveira RV, Cruz LP, Matos MA. Comparative accuracy assessment of the Gustilo and Tscherne classification systems as predictors of infection in open fractures. Rev Bras Ortop 2018;53:314-8. [Crossref] [PubMed]
- Weston JT, Liu X, Wandtke ME, et al. A systematic review of total dislocation of the talus. Orthop Surg 2015;7:97-101. [Crossref] [PubMed]
- Hagebusch P, Neun O, Gramlich Y, et al. Open Ankle Dislocation without Associated Malleolar Fracture on a Trampoline. A Case Report. Z Orthop Unfall 2020;158:347-51. [Crossref] [PubMed]
- Shen LF, Zhang C, Guo QF, et al. Application of damage control in severe traumatic limb salvage. Zhongguo Gu Shang 2012;25:152-4. [PubMed]
- Buckley RE, Moran CG, Apivatthakakul T. AO Principles of Fracture Management. New York, NY, USA: Thieme, 2017.
- Al-Obaidi B, Wiik AV, Bhattacharyya R, et al. Fibular nails for open and closed ankle fractures: Results from a non-designer level I major trauma centre. J Orthop Surg (Hong Kong) 2019;27:2309499019832420. [Crossref] [PubMed]
- Xiao BP, Li M, Mao WM, et al. Therapeutic strategies of grade-III open fractures of tibia and fibula. Zhongguo Gu Shang 2008;21:289-90. [PubMed]
Cite this article as: Talesa GR, Mercurio M, Castioni D, Ceccarini P, Antinolfi PL, Di Giacomo LM, Rinonapoli G, Caraffa A. Early total care for open lateral ankle dislocation without tearing of tibiofibular sindesmosis: case report. J Xiangya Med 2022;7:30.