Estimation of sodium and potassium intake level from spot urine samples among urban adults in Bangladesh
Highlight box
Key findings
• The daily estimated salt intake from spot urine was much higher (9.6 grams/day) than the recommended level among the urban community people.
• Women and added salt while having meal were associated with high salt consumption.
• The estimated potassium intake was much lower than the recommended level and the mean sodium/potassium ratio was nearly five times higher that the World Health Organization recommendation.
What is known and what is new?
• Salt consumption among Bangladeshi population is higher.
• The daily estimated salt intake among the urban community people was almost double (9.6 grams/day) to the recommended level and, women and added salt were associated with high salt consumption.
What is the implication, and what should change now?
• Despite having greater access to health education, urban residents consume more salt than the recommended level. Therefore, further evidence relating to dietary patterns, sources of salt, salt sensitivity, and the effects of educational programme among urban populations is required.
Introduction
Salt consumption, especially its generic component ‘sodium (Na+)’, has been an interest in public health nutrition for decades due to its adverse impact on cardiovascular health (1). Considering its importance, reducing Na+ intake has emerged as a leading target to halt the ongoing mortality from cardiovascular disease. Conversely, high potassium (K+) intake is protective for cardiovascular health through an indirect beneficial effect on blood pressure (2). Recent evidence reported a new method to seek the impact of these two (Na+ and K+) on cardiovascular health, the sodium-to-potassium ratio (Na+/K+). This promising ratio has already emerged as a risk factor for stroke, cardiovascular disease, and all-cause mortality in longitudinal studies (3,4). However, if an individual consumes Na+ and K+ as recommended, the Na+/K+ ratio would be approximately one to one, which is considered beneficial for health (5). Thus the combination of increased potassium and decreased sodium intake favorably alter their ratio which can be effective in reducing adverse cardiovascular health outcomes, mortality, and medical expenses (6,7).
Although a large body of research conducted in this area, there are divergent interpretations of available data, with some advocating a re-evaluation of the current guideline recommendations or methods of estimation (8,9). This is because the findings of Na+ and K+ intake about adverse health outcomes are inconsistent throughout the world. One of the major causes of these inconsistencies is variations in methods of measuring these two. While guidelines are recommending healthy intake based on the clinical trials using 24-hour urinary excretion, most of the population-based surveys have used dietary recall methods to assess that makes the data incomparable (8,10). Again, some criticized 24-hour urinary measurement as an impractical method for population survey and limited by the high costs, high burden, the recently demonstrated inaccuracies and risk of collection errors (9), especially for low resource countries where these limitations underscore the importance of such method. Hence, for these countries, an alternative but comparable method is recommended.
In Bangladesh, data on Na+ and K+ intake, and their ratio are insufficient and limited by study design, measurement method, and generalizability. However, irrespective of these limitations, available studies mostly focused on salt consumption and reported it is much higher than recommended level (>5 grams) among Bangladeshi adults (11-15). Among these, only two studies reported mean Na+ intake as 6,555 mg/day (285 mmol/day or 16.8 gram salt/day) using spot urine among urban adults (12) and 2,652 mg/day (115 mmol/day or 6.8 gram salt/day) among coastal adults using a single 24-h urine sample (11). The most recent national survey also reported high Na+ intake which was 3,519 mg/day (153 mmol/day or 9 gram salt/day) amongst 18–69 years adults with a minimal urban-rural difference (16,17). As per our knowledge, no study was conducted in Bangladesh to estimate K+ intake and evaluate the Na+/K+ ratio. Hence, considering the lack of evidence and comparable method. This study aimed at estimating the Na+ and K+ intake and evaluating their ratio among urban Bangladeshi adults using spot urine samples. Besides, the salt consumption and its potential determinants were also assessed as an adjunct to the above measurement. We present this article in accordance with the STROBE reporting checklist (available at https://jxym.amegroups.com/article/view/10.21037/jxym-23-12/rc).
Methods
Study place and population
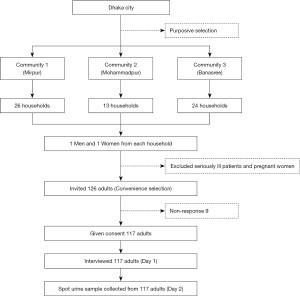
A community-based cross-sectional study was conducted in three selected areas (Mirpur, Mohammadpur, and Banasree) of Dhaka city having similar socioeconomic background. Adults (≥18 years and both genders) residing in these three areas were the study population. A total of 117 men and women from 63 households (26 from Mirpur, 13 from Mohammadpur, and 24 from Banasree) were approached using the convenience sampling technique. Two persons (one man and one woman) from each household were targeted. We excluded those who were seriously ill and pregnant (Figure 1). The study period was from September 2020 to November 2020.
Data collection procedures
The investigators’ general message was given to all the adult family members of the respective buildings regarding the study purpose and voluntary participation. One adult man and one woman from each family were invited for an interview and urine sample collection. Then the available participants were interviewed and at least two visits were made for each missed person. Information on dietary salt intake, history of medication for diabetes, and hypertension were asked following informed written consent. After those anthropometric measurements were completed. The height was measured (in centimeters) without shoes by using a measuring tape attached to the wall. Then weight was measured by the portable weighing scale in kilogram (kg) after removal of their footwear and heavy clothing. Body mass index (BMI) was calculated as weight in kg/(height in meter)2.
Procedures for spot urine collection
A 20 mL sterile labeled container was supplied to the subjects to collect their urine for a ‘spot’ urine specimen after explaining the proper urine preservation technique. All specimens were asked to store overnight at normal temperature. The researcher collected the sample in the morning and sent it to the laboratory for analysis. An ion-selective electrode method was used for the estimation of urinary sodium and electrolytes (15,18). Participants were instructed to collect the last void urine of the day. The containers were labeled with the patient’s name and a unique identifier number, date, and time of collection was mentioned (16).
Equation for estimating 24-hour Na+ and K+ excretion from spot urine sample
To estimate 24-hour urinary Na+, K+ and Na+/K+ ratio in this study, we used the Tanaka equation (18). Tanaka et al. developed this equation to estimate 24-hour urinary Na+ and K+ excretion, using Japanese data items from the INTERSALT study, which was conducted through a highly standardized method (18). They developed this equation by comparing both 24-hour urine samples and spot urine on the same subjects. Age, sex, weight, and height of the respondents, and creatinine were the additional information that was used to formulate the equation. After applying that, we calculated 24-hour sodium intake, which is then converted to salt intake by the division of 17.1 as a conversion factor to attain the estimated salt intake in grams (19).
Ethical issues
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and we assured that the data would be used for scientific research only. This study was approved by the ethical review committee of the Bangladesh University of Health Sciences (memo No. BUHS/ERC/EA/20/242). Written informed consent was obtained from all the patients before taking part in the study.
Statistical analysis
The data were entered in an Excel spreadsheet and logical checks were done to check for any kind of inconsistency. All missing data was excluded from the analysis. Statistical analyses were performed with Statistical Package for the Social Sciences for Windows, version 26. Continuous variables are shown as the mean (± standard deviation) and categorical variables were shown as n (%). To show the distribution of urinary Na+ and K+ excretion, we also used error bars using the mean (± standard deviation). Differences of categorical and quantitative variables across groups were compared using the Chi-square test and t-test respectively. A saturated model of binary logistic regression was used to assess the potential determinants of high salt intake (≥5 grams/day) where all the possible variables were included according to the rules of variable selection in regression (20,21). Prior to running the regression, the following assumptions were checked: multicollinearity, outlier, and the independence of observations. We did not find any violation of these assumptions. All the estimates of precision were presented at a 95% confidence interval (CI), and the statistical tests were considered significant (2-tailed) at a level of P<0.05.
Results
Background characteristics of the participants
Of the 117 participants, the mean (± standard deviation) age was 42.8 (±11.8) years, and most (70.1%) of the participants graduated. Their mean BMI was 25.2 (±4.6) kg/m2. The self-reported prevalence of hypertension and diabetes was 22.2% and 31.6% respectively. Nearly one-third (29.9%) of them used to add salt (1.6±0.8 grams/day) and more than one-third (35%) practice restricting salt intake while taking meals (Table 1).
Table 1
| Characteristics | Total (n=117) | Men (n=58) | Women (n=59) | P |
|---|---|---|---|---|
| Age, years, mean ± SD | 42.8±11.8 | 45.9±11.9 | 39.7±10.9 | <0.001 |
| Age groups, years, n (%) | 0.31 | |||
| 18–44 | 70 (59.8) | 32 (55.2) | 38 (64.4) | |
| 45–69 | 47 (40.2) | 26 (44.8) | 21 (35.6) | |
| Education levels, n (%) | <0.001 | |||
| Below graduation | 35 (29.9) | 10 (17.2) | 25 (42.4) | |
| Graduation and above | 82 (70.1) | 48 (82.8) | 34 (57.6) | |
| Body mass index, kg/m2, mean ± SD | 25.2±4.6 | 24.2±3.1 | 26.2±5.5 | 0.02 |
| Occupation, n (%) | <0.001 | |||
| Business | 17 (14.5) | 15 (25.9) | 2 (3.4) | |
| Government and private service | 44 (37.6) | 32 (55.2) | 12 (20.3) | |
| Household work | 39 (33.3) | 0 | 39 (66.1) | |
| Retired, student, unemployed | 17 (14.5) | 11 (19.0) | 6 (10.2) | |
| Self-reported hypertension, n (%) | 26 (22.2) | 15 (25.9) | 11 (18.6) | 0.35 |
| Self-reported diabetes, n (%) | 37 (31.6) | 20 (34.5) | 17 (28.8) | 0.51 |
| Use added salt while eating a meal, n (%) | 35 (29.9) | 13 (22.4) | 22 (37.3) | 0.08 |
| Always or often used added salt, n (%) | 16 (45.7) | 7 (53.8) | 9 (40.9) | 0.46 |
| Amount of salt (g/day) added while eating a meal, mean ± SD | 1.6±0.8 | 1.9±1.2 | 1.4±0.0 | 0.09 |
| Currently taking measures to control salt intake, n (%) | 41 (35.0) | 18 (31.0) | 23 (39.0) | 0.37 |
SD, standard deviation.
Estimated 24-hour urinary Na+ and K+ excretion, and their ratio
The mean Na+ and K+ excretion (mmol/L) was 71.5 (95% CI: 44.6–98.4) and 17.8 (95% CI: 9.5–26.2) respectively while directly measured from the spot urine. Using the Tanaka equation, the estimated mean of 24-hour urinary Na+ and K+ excretion (mmol/L) was 164.1 (154.4–173.8) and 38.3 (35.0–41.6) respectively. The overall mean of Na+/K+ ratio was 4.5 (95% CI: 4.3–4.7) without any mentionable difference in sex (Table 2). A high percentage of participants did not meet the World Health Organization (WHO) recommendation as 89.7% for Na+ excretion, 99.1% for K+ excretion and 100% for Na+/K+ ratio. These percentages were higher among the younger age groups (18–44 years) and those who did not add salt to meals (Table 3).
Table 2
| Variables | Total (n=117) | Men (n=58) | Women (n=59) |
|---|---|---|---|
| Measured component of spot urine | |||
| Sodium, mmol/L | 71.5 (44.6–98.4) | 65.2 (31.4–99.0) | 77.63 (60.2–95.0) |
| Potassium, mmol/L | 17.8 (9.5–26.2) | 16.6 (9.4–23.8) | 19.05 (9.8–28.3) |
| Creatinine, mg/dL | 62.4 (41.7–82.9) | 72.3 (61.5–83.1) | 52.55 (11.5–93.6) |
| Chloride, mmol/L | 76.9 (41.2–112.7) | 69.4 (24.9–113.9) | 84.34 (58.0–110.7) |
| Estimated 24-hour urinary sodium excretion (mmol/L)† | 164.1 (154.4–173.8) | 151.4 (115.5–187.4) | 176.5 (127.5–225.6) |
| Estimated 24-hour urinary potassium excretion (mmol/L)† | 38.3 (35.0–41.6) | 35.9 (31.4–40.4) | 40.7 (35.8–45.6) |
| Estimated 24-hour urinary sodium-potassium ratio | 4.5 (4.3–4.7) | 4.5 (4.2–4.7) | 4.6 (4.3–4.9) |
†, using Tanaka et al. (18) equation:
UrNa, 24-h urinary sodium; NaSpot, Na concentration in the spot voiding urine; CrSpot, creatinine concentration in the spot voiding urine; PrUCr24h, predicted value of 24 hours urine creatinine; UrK, 24-h urinary potassium; K Spot, K concentration in the spot voiding.
Table 3
| Characteristics | N | Na+, mmol/day | K+, mmol/day | Na+/K+ ratio | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (95% CI) | >85†, % (95% CI) | Mean (95% CI) | <90†, % (95% CI) | Mean (95% CI) | >1†, % (95% CI) | ||||
| All | 117 | 164.1 (151.6–176.6) | 89.7 (84.2–95.2) | 38.3 (35.0–41.6) | 99.1 (97.4–100) | 4.5 (4.3–4.7) | 100 (100.0–100.0) | ||
| Age group, year | |||||||||
| 18–44 | 70 | 167.5 (149.9–185.2) | 59.0 (50.1–67.9) | 37.6 (33.2–42.0) | 59.5 (50.6–68.4) | 4.6 (4.4–4.9) | 59.8 (50.9–68.7) | ||
| 45–69 | 47 | 158.9 (141.8–176.3) | 41.0 (32.1–49.9) | 39.5 (34.3–44.4) | 40.5 (31.6–49.4) | 4.3 (3.9–4.6) | 40.2 (31.3–49.1) | ||
| Education | |||||||||
| Below graduation | 35 | 166.7 (145.7–187.7) | 30.5 (22.2–38.8) | 40.5 (34.3–46.6) | 30.2 (21.9–38.5) | 4.3 (4.0–4.7) | 29.9 (21.6–38.2) | ||
| Graduation and above | 82 | 162.9 (147.3–178.6) | 69.5 (61.2–77.8) | 37.4 (33.4–41.4) | 69.8 (61.5–78.1) | 4.6 (4.4–4.6) | 70.1 (61.8–78.4) | ||
| Added salt while eating a meal | |||||||||
| Yes | 35 | 166.6 (152.4–180.9) | 30.5 (22.2–38.8) | 34.3 (28.1–40.5) | 29.3 (21.1–37.5) | 4.9 (4.4–5.3) | 29.9 (21.6–38.2) | ||
| No | 82 | 158.2 (132.1–184.2) | 69.5 (61.2–77.8) | 40.0 (36.1–43.9) | 70.7 (62.5–78.9) | 4.4 (4.1–4.7) | 70.1 (61.8–78.4) | ||
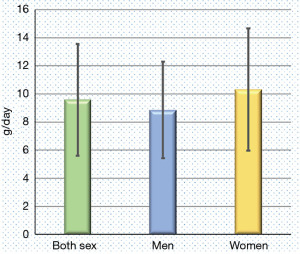
Estimated 24-hour urinary salt excretion
The mean (± standard deviation) estimated 24-h urinary salt excretion was 9.6 (±4) grams/day and it was higher among women than men (10.5±4.4 versus 8.8±3.4 grams/day) (Figure 2). Most of the participants (88.9%) consumed more than recommended (>5 grams/day) level of salt (data not presented).
Determinants of high salt intake
In case of the factors that determined the high salt intake among the study population, women and added salt intake showed higher odds ratio (OR >1) for high salt consumption (≥5 grams/day) (Table 4).
Table 4
| Factors | Adjusted odds-ratio | 95% confidence interval for odds-ratio | |
|---|---|---|---|
| Lower | Upper | ||
| Gender (Ref. men) | 2.095 | 0.572 | 7.672 |
| Added salt intake (Ref. no) | 1.055 | 0.243 | 4.585 |
| Salt reduction important (Ref. no) | 0.523 | 0.053 | 5.114 |
| Practice to control salt intake (Ref. no) | 0.465 | 0.124 | 1.734 |
| Hypertensive (Ref. no) | 0.355 | 0.050 | 2.526 |
| Diabetic (Ref. no) | 0.639 | 0.133 | 3.083 |
Discussion
Salt intake estimation studies are sparse in Bangladesh. Similarly, it is true for the Na+ and K+ intake, and their ratio. In this perspective, we assumed our current estimations using spot urine are more convenient and valid estimates, and report here that a high percentage of participants did not meet the WHO recommendation (2,22) for Na+ and K+ intake, and Na+/K+ ratio.
Based on the current study using spot urine, urban community residents of Dhaka city used to take 164.1 mmol/L (3.8 gram/day) of Na+ daily which is higher than the other Asian countries including Malaysia (23), Singapore (24), Thailand (25,26), Indonesia (27) and Vietnam (28,29). Again, some other countries reported higher sodium intake than the current study (3,774 milligrams/day): India (4,098 mg/day in Andhra Pradesh); South Korea (3,960 mg/day); China (4,349 mg/day); Nepal (5,280 mg/day) (30-33). In Bangladesh, the findings are inconsistent for three available studies (11,12,16,17). Among these, a recent nationally representative survey in Bangladesh and an individual study in the coastal region showed comparatively less Na+ intake than the current estimation (16,17). However, another Bangladeshi study (12) reported a higher intake than the current one. In combination, all of the Bangladeshi studies reported higher intake than the recommended (2,22) as same as the current study. Naser et al. provide values for 24-hour urinary sodium excretion when determined directly and when estimates from spot urine sodium measurements were derived using the Kawasaki, Tanaka, or INTERSALT formulae. Results from all formula-based estimations were skewed, with mean skewed values of 230, 1,035, and 1,196 mg/24 hours (34,35).
The estimated mean K+ intake among the study population is 38.3 mmol/L (1,493 milligrams or 1.5 gram/day) per day which is much lower than the WHO recommendation (2). This estimation is also much lower than the other countries including Japan, Iran, and South Korea (36-38). Again, in this study, high Na+ and low K+ intake badly impact their ratio (mean Na+/K+ ratio 4.5) which is nearly five times higher than the WHO recommendation (2). This estimation is much higher than the Na+/K+ ratio of other countries including Iran (3.69) and South Korea (1.88 to 1.71) (39,40), and similar to the findings of Thailand (5 times higher) (26).
Our study elucidated that the daily consumption of salt in an urban sample of Dhaka is 9.6 grams/day. Interestingly, our finding using spot urine is similar to the national (9 grams/day) (16,17), and global (10.06 grams/day) estimation of salt intake (41). Our finding of salt intake is also supported by the studies of developed countries where the estimated salt intake range from 9·2 to 10.6 grams/day irrespective of the methods applied (41,42). Our estimation using the Tanaka equation is also supported by the neighboring country India where the mean estimated salt intake was 9.04 grams/day and 9.79 grams/day for Delhi and Haryana, and Andhra Pradesh respectively (30).
In this study, most of the participants did not meet the WHO recommendation of Na+, K+ and salt intake: Na+ excretion (89.7%); K+ excretion (99.1%); Na+/K+ ratio (100%); and salt excretion (88.9%). These findings are supported by global data for Na+ intake, K+ intake, Na+/K+ ratio, and salt consumption (43-45). Again, we identified that women participants are more likely to consume excess Na+, K+, and dietary salt. In Bangladesh, similar sex difference was also elucidated by another study (11) for salt consumption and possibility included the participation of more housewives who have more access to add salt during cooking or mealtime. This explanation is also applicable for excess Na+ intake among the women participants as it is the generic component of salt (1,46). The aforementioned discussion regarding the gender is also supported that female is a determinant of high salt intake for Bangladeshi urban adults. However, a previous study contradicts this finding in term of determinants (47). We found more Na+ and salt consumption among the younger age group and more K+ intake among the older age groups which are consistent with the national survey in Bangladesh (16) for salt intake and the Minnesota Heart Survey (42) for K+ intake. The young group of people consumed more salt as they have habits of eating more processed food or eating outside the home (33). On the other hand, the older group restricts themselves due to comorbidities (such as hypertension and diabetes) or advice from doctors.
In the current study, self-reported added salt intake was nearly one-third of the total participants that coincides with the previous study in Bangladesh (13). We found the urinary salt excretion is higher among those who claimed that they did not add extra salt while taking a meal or adding it during cooking. Nevertheless, this added salt intake (OR 1.055) appeared to be a determinant of high salt consumption in the current study and was supported by an Indian population-based study (44). However, 24-hour urinary salt excretion contradicts this subjective assessment as 88.9% of the participants exceeded the recommended level (>5 grams/day) of salt intake. This is why the measurement method is an important issue to assess population-level Na+, K+, and salt intake, and a subjective approach may misguide national policy recommendations. Other than the method, here the self-reported statement of salt intake represented only the amount that participants used to add while cooking or eating a meal. This is a portion of total daily salt intake that did not consider the other sources of dietary salt. This finding suggests modifying the public health message that mostly advises by clinicians to avoid salt while eating or cooking. Hence, policymakers should consider other sources of dietary salt along with added salt while recommending intervention to reduce the population-level total salt consumption.
Overall, inconsistent findings exist globally regarding Na+ intake, K+ intake, Na+/K+ ratio and salt intake. This variation among the Bangladeshi urban population and other developed or developing countries could be explained in the light of dietary sources. In this regard, a systematic review stated that countries undergoing epidemiological transition also facing a nutritional transition that is prone to the entire population toward widespread availability of energy-dense foods rich in salt and its component sodium (47). Thus the dietary pattern has shifted from a reliance on traditional food items (fruits, vegetables rich in K+) to the salt-rich processed food that is contributing to increasing population-level dietary salt and sodium consumption. In this regard, a comprehensive review postulated several evidence-based reasons for such inconsistency like (I) variations in methods of measuring sodium intake; (II) variations in population characteristics; (III) dietary pattern; (IV) salt sensitivity; and (V) study design (8).
The main strength of this study is the simultaneous measurement of Na+ and K+ intake, their ratio, and salt intake using spot urine in urban community settings. Again, simultaneous application of both subjective and objective assessment on the same population elucidated the real scenario of community-level consumption (Na+, K+, and salt) and related behaviors. Besides, this study assessed the potential determinants of high salt intake for a typical urban adult population. As per our knowledge, such evidence is currently lacking in Bangladesh that will guide future research in a similar setting.
On the other hand, convenience selection of study areas and samples due to the coronavirus 2019 pandemic limits the generalizability of the study findings. Moreover, we did not adjust our findings for energy intake and losses of Na+ and K+ other than the urinary tract. As a result, sex-specific findings may not be accurately estimated, and the excretion of Na+ and K+ may not be comparable to other countries where these adjustments are taken into consideration.
Conclusions
In conclusion, analysis of spot urine samples revealed the majority of the urban community people are habituated to consuming high Na+ and low K+. Though small sample size and lack of adjustments for energy intake and Na+/K+ excretion limits generalizability of study findings. Hence, the findings suggest, women and those used to add salt while taking a meal are the primary target of intervention to bring favorable changes in the daily intake of Na+ and K+ in an urban setting.
Acknowledgments
We acknowledge everyone who participated in this study, also acknowledge the Bangladesh Medical Research Council for the funding.
Funding: Bangladesh Medical Research Council (BMRC), grant number: BMRC/RP/Revenue/2019-2020/607/6-98.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jxym.amegroups.com/article/view/10.21037/jxym-23-12/rc
Data Sharing Statement: Available at https://jxym.amegroups.com/article/view/10.21037/jxym-23-12/dss
Peer Review File: Available at https://jxym.amegroups.com/article/view/10.21037/jxym-23-12/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jxym.amegroups.com/article/view/10.21037/jxym-23-12/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the ethical review committee of the Bangladesh University of Health Sciences (memo No. BUHS/ERC/EA/20/242). Written informed consent was taken from all the patients before taking part in the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Aburto NJ, Ziolkovska A, Hooper L, et al. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ 2013;346:f1326. [Crossref] [PubMed]
- World Health Organization. Guideline: Potassium intake for adults and children. Geneva: WHO; 2012.
- Mirmiran P, Bahadoran Z, Nazeri P, et al. Dietary sodium to potassium ratio and the incidence of hypertension and cardiovascular disease: A population-based longitudinal study. Clin Exp Hypertens 2018;40:772-9. [Crossref] [PubMed]
- Okayama A, Okuda N, Miura K, et al. Dietary sodium-to-potassium ratio as a risk factor for stroke, cardiovascular disease and all-cause mortality in Japan: the NIPPON DATA80 cohort study. BMJ Open 2016;6:e011632. [Crossref] [PubMed]
- World Health Organization. Diet, nutrition and the prevention of chronic disease. Report of a Joint WHO/FAO Expert Consultation. Geneva: WHO; 2003.
- Chang HY, Hu YW, Yue CS, et al. Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. Am J Clin Nutr 2006;83:1289-96. [Crossref] [PubMed]
- Kawasaki T, Itoh K, Kawasaki M. Reduction in blood pressure with a sodium-reduced, potassium- and magnesium-enriched mineral salt in subjects with mild essential hypertension. Hypertens Res 1998;21:235-43. [Crossref] [PubMed]
- O'Donnell MJ, Mente A, Smyth A, et al. Salt intake and cardiovascular disease: why are the data inconsistent? Eur Heart J 2013;34:1034-40. [Crossref] [PubMed]
- Ginos BNR, Engberink RHGO. Estimation of Sodium and Potassium Intake: Current Limitations and Future Perspectives. Nutrients 2020;12:3275. [Crossref] [PubMed]
- Kawasaki T, Itoh K, Uezono K, et al. A simple method for estimating 24 h urinary sodium and potassium excretion from second morning voiding urine specimen in adults. Clin Exp Pharmacol Physiol 1993;20:7-14. [Crossref] [PubMed]
- Rasheed S, Jahan S, Sharmin T, et al. How much salt do adults consume in climate vulnerable coastal Bangladesh? BMC Public Health 2014;14:584. [Crossref] [PubMed]
- Zaman MM, Choudhury SR, Ahmed J, et al. Salt Intake in an Adult Population of Bangladesh. Glob Heart 2017;12:265-6. [Crossref] [PubMed]
- Zaman MS, Barua L, Bushra S, et al. Salt Intake Behavior Among the Faculties And Doctors of Bangladesh University of Health Sciences. Cardiovasc J 2016;8:94-8. [Crossref]
- Mondal R, Sarker RC, Chandra Banik P. Knowledge attitude and behaviour towards dietary salt intake among Bangladeshi medical and nonmedical undergraduate students. International Journal of Perceptions in Public Health 2017;2:31-7. [Crossref]
- Mondal R, Sarker RC, Sayrin R, et al. Knowledge, Attitude and Practice towards Dietary Salt Intake among Nurses Working in a Cardiac Hospital in Bangladesh Sciences. Cardiovasc J 2019;12:53-8. [Crossref]
- World Health Organization. Country Office for Bangladesh. (2018). National STEPS survey for non-communicable diseases risk factors in Bangladesh 2018. World Health Organization. Country Office for Bangladesh. Accessed February 10, 2021. Available online: https://apps.who.int/iris/handle/10665/332886
- Riaz BK, Islam MZ, Islam ANMS, et al. Risk factors for non-communicable diseases in Bangladesh: findings of the population-based cross-sectional national survey 2018. BMJ Open 2020;10:e041334. [Crossref] [PubMed]
- Tanaka T, Okamura T, Miura K, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens 2002;16:97-103. [Crossref] [PubMed]
- World Health Organization. WHO STEPS surveillance manual: the WHO STEPwise approach to chronic disease risk factor surveillance. Geneva: WHO; 2005.
- Bendel RB, Afifi AA. Comparison of Stopping Rules in Forward "Stepwise" Regression. J Am Stat Assoc 1977;72:46-53.
- Costanza MC, Afifi AA. Comparison of stopping rules in forward stepwise discriminant analysis. J Am Stat Assoc 1979;74:777-85. [Crossref]
- World Health Organization. Guideline: Sodium intake for adults and children. Geneva: WHO; 2012.
- Mirnalini K Jr, Zalilah MS, Safiah MY, et al. Energy and Nutrient Intakes: Findings from the Malaysian Adult Nutrition Survey (MANS). Malays J Nutr 2008;14:1-24. [PubMed]
- Health Promotion Board, Singapore. Report of the National Nutrition Survey 2010. Singapore: Research and Strategic Planning Division; 2010.
- Supornsilaphachai C. Evolution of salt reduction initiatives in Thailand: lessons for other countries in the South-East Asia Region. WHO Regional Health Forum 2013;17:61-71.
- Chailimpamontree W, Kantachuvesiri S, Aekplakorn W, et al. Estimated dietary sodium intake in Thailand: A nationwide population survey with 24-hour urine collections. J Clin Hypertens (Greenwich) 2021;23:744-54. [Crossref] [PubMed]
- Gunung IK. Iodine level of iodized salt required in endemic area. 2008. Accessed 9 July 2021. Available online: https://ojs.unud.ac.id/index.php/ijbs/article/view/3742php?article=14366&val=965
- Do HTP. Hypertension in Vietnam: prevalence, risk groups and effects of salt substitution. Netherlands: Wageningen University; 2014.
- Tran TM, Komatsu T, Nguyen TK, et al. Blood pressure, serum cholesterol concentration and their related factors in urban and rural elderly of Ho Chi Minh City. J Nutr Sci Vitaminol (Tokyo) 2001;47:147-55. [Crossref] [PubMed]
- Johnson C, Mohan S, Rogers K, et al. Mean Dietary Salt Intake in Urban and Rural Areas in India: A Population Survey of 1395 Persons. J Am Heart Assoc 2017;6:e004547. [Crossref] [PubMed]
- Rhee MY, Shin SJ, Park SH, et al. Sodium intake of a city population in Korea estimated by 24-h urine collection method. Eur J Clin Nutr 2013;67:875-80. [Crossref] [PubMed]
- Tan M, He FJ, Wang C, et al. Twenty-Four-Hour Urinary Sodium and Potassium Excretion in China: A Systematic Review and Meta-Analysis. J Am Heart Assoc 2019;8:e012923. [Crossref] [PubMed]
- Neupane D, Rijal A, Henry ME, et al. Mean dietary salt intake in Nepal: A population survey with 24-hour urine collections. J Clin Hypertens (Greenwich) 2020;22:273-9. [Crossref] [PubMed]
- Naser AM, He FJ, Rahman M, et al. Spot urine formulas to estimate 24-hour urinary sodium excretion alter the dietary sodium and blood pressure relationship. Hypertension 2021;77:2127-37. [Internet]. [Crossref] [PubMed]
- Whelton PK. Sodium, blood pressure, and cardiovascular disease. Hypertension 2021;77:2138-9. [Crossref] [PubMed]
- Okuda N, Okayama A, Miura K, et al. Food Sources of Dietary Potassium in the Adult Japanese Population: The International Study of Macro-/Micronutrients and Blood Pressure (INTERMAP). Nutrients 2020;12:787. [Crossref] [PubMed]
- Mirzaei M, Soltaniz M, Namayandeh M, et al. Sodium and potassium intake of urban dwellers: nothing changed in Yazd, Iran. J Health Popul Nutr 2014;32:111-7. [PubMed]
- Lee HS, Duffey KJ, Popkin BM. Sodium and potassium intake patterns and trends in South Korea. J Hum Hypertens 2013;27:298-303. [Crossref] [PubMed]
- Powles J, Fahimi S, Micha R, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013;3:e003733. [Crossref] [PubMed]
- Global Status Report on Noncommunicable Diseases 2014: Attaining the Nine Global Noncommunicable Diseases Targets, a Shared Responsibility. Geneva: World Health Organization; 2014.
- Land MA, Webster J, Christoforou A, et al. Salt intake assessed by 24 h urinary sodium excretion in a random and opportunistic sample in Australia. BMJ Open 2014;4:e003720. [Crossref] [PubMed]
- van Mierlo LA, Greyling A, Zock PL, et al. Suboptimal potassium intake and potential impact on population blood pressure. Arch Intern Med 2010;170:1501-2. [Crossref] [PubMed]
- Sodium intakes around the world. Background document prepared for the Forum and Technical meeting on Reducing Salt Intake in Populations (Paris 5–7 October 2006). Geneva: World Health Organization; 2007.
- Petersen KS, Johnson C, Mohan S, et al. Estimating population salt intake in India using spot urine samples. J Hypertens 2017;35:2207-13. [Crossref] [PubMed]
- Webster J, Su'a SA, Ieremia M, et al. Salt Intakes, Knowledge, and Behavior in Samoa: Monitoring Salt-Consumption Patterns Through the World Health Organization's Surveillance of Noncommunicable Disease Risk Factors (STEPS). J Clin Hypertens (Greenwich) 2016;18:884-91. [Crossref] [PubMed]
- Johnson C, Mohan S, Rogers K, et al. The Association of Knowledge and Behaviours Related to Salt with 24-h Urinary Salt Excretion in a Population from North and South India. Nutrients 2017;9:144. [Crossref] [PubMed]
- Menyanu E, Russell J, Charlton K. Dietary Sources of Salt in Low- and Middle-Income Countries: A Systematic Literature Review. Int J Environ Res Public Health 2019;16:2082. [Crossref] [PubMed]
Cite this article as: Omi FR, Bhuiyan R, Shraboni NN, Barua L, Banik PC, Faruque M, Zaman MM. Estimation of sodium and potassium intake level from spot urine samples among urban adults in Bangladesh. J Xiangya Med 2023;8:7.